The Efficacy of Tranexamic Acid in Reduction of Blood Loss in Femur Surgery: A Randomized Controlled Study
Author'(s): Daddy H1*, Gagara M1, Chaïbou MS1, Mahamadou OR1, James Didier L2 and Garba I2
1Department of Anesthesia, Niamey National Hospital, Niger
2Department of Surgery, Niamey National Hospital, Niger
*Correspondence:
Dr. Daddy Hadjara, Anesthesia Department, Niamey National Hospital.
Received: 17 February 2020; Accepted: 05 March 2020
Citation: Daddy H, Gagara M, Chaïbou MS and al. The Efficacy of Tranexamic Acid in Reduction of Blood Loss in Femur Surgery: A Randomized Controlled Study. Anesth Pain Res. 2020; 4(1): 1-6.
Abstract
Aims: This study aimed to study the efficacy of tranexamic acid (TXA) for reduction of blood loss in femur surgery.
Methods: This study design was a prospective randomized controlled double-blind study, from March 25th, 2019 to September 24th, 2019. Fifty-six (56) patients aged from 18 to 45 years, that underwent femur surgery, classed American Society of anesthesiologist I status were randomized into 2 groups. The first group received TXA in 50 cc of normal saline (group TXA) compared to control group Control (group C), 38 patients received 50 cc normal saline alone. Statistical Analysis used: Pearson khi² test, the Fisher test and Student test with P Value Ë‚5%.
Results: Fifty-six (56) patients randomized in two groups (TXA and C) of 28 patients. Demographic, clinical and paraclinical characteristics were the same in the two groups (p=ns). The average age was 27.79 years in group TXA versus 29.64 years in group C(p=0.045). Comparative study between the 2 groups revealed significant decrease of estimated blood loss (p=0.045) as well as a significant gain of final hemoglobin rate (p=0.009). There was no significative difference for blood transfusion (p=0.11).
Conclusion: Tranexamic acid significantly decreases the blood loss in femur surgery and has a gain on the final hemoglobin.
Keywords
Introduction
Femoral surgery is considered as potentially hemorrhagic. Blood saving is the main preoccupation in peri-operative period. Multiple methods are used to reduce blood loss, including the use of tranexamic acid, a lysine’s analogue antifibrinolytic [1]. In developing countries, traumatic surgery is a concern because of the development of the car fleet. Erythropoietin stimulation, hemodilution and above all autologous transfusion are the main methods used to correct anemia in peri-operative period. However, labile blood products are not always available, hence the interest of this study on the efficacity of tranexamic acid in reducing blood loss during peri and post-operative period in order to propose this alternative in the management of anemia [2].
Patients and Methods
This study is a prospective, randomized, single-blind, placebo- controlled trial case-control study conducted from March 25th, 2019 to September 24th, 2019 in the department of anesthesia of Niamey National hospital. The study was approved by faculty of medicine, Abdou Moumouni University of Niamey and obtaining an informed consent from the patients. The choice of groups was kept confidential by the investigator and was not mentioned on the patient's file. Patients were followed 30 days after surgery.
Inclusion criteria included 56 patients aged 18-45-year-old, both sexes, undergoing femur traumatic surgery classed American Society of anesthesiologist I status. The patients were randomized into two groups (28 patients in each group).
Tranexamic acid group (group TXA), 28 patients were given 20 min before the surgical incision 1g of tranexamic acid in 50 cc of isotonic saline, another dose of 1g three hour after. Control group (group C) 28 patients were given 50 cc normal saline where been considered the epidemiological, clinical, paraclinical aspects, blood loss, hemoglobin and transfusion were. Data were analyzed with Epi Info 7TM (Center for Disease Control and Prevention, Atlanta, GA), Pearson Khi2 and Fisher tests. As for quantitative variables, we used Student test. Significatively threshold was fixed for p<0.05.
Results
Fifty-six (56) patients were included and were randomly divided into two group, and each group has 28 patients. The prevalence of femur fracture was 24.12% and the incidence of patients that were classed ASA-I, 23%. As regarding demographic data; comparative study between the 2 groups revealed non-significant difference in the two groups (p=ns). The average age was 27.79 years in group TXA vs 29.64 years in group C (p=0.59) and Body Mass Index in TXA group was 23.53 ± 2.02kg/m2 and 23.84 ± 3.97kg/m2 in group C(p=0.20). The average delay of the surgery was 49.86 ±76.74 days in group TXA and 217.84 ± 365.20 days for the control (p=0.019) (Table 1). The circumstances of the femur fracture were road traffic injury in 96.64% of the patients, followed by ballistic trauma in 3.57%, domestic accidents with 1.79%.
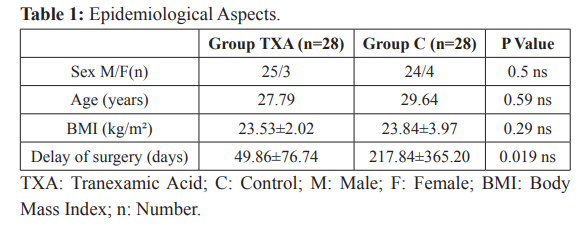
The indication of surgery was femoral diaphysis in 69.64% of the cases. For thromboembolic prevention, 13 patients (23.21%) in group TXA versus 7 patients (12.5%) in group C received enoxaparin in pre-operative period. Spinal anesthesia was performed in 92.86%, and general anesthesia in 7.14%. The average duration time of the surgery was 72.86 ± 23.12min in group TXA and 82.68 ± 48.98min for the control group (p=0.11). The average of blood loss in peri-operative was 720 ± 436.49ml in group TXA; 813.57 ± 580.92ml for control group (p=0.31). Blood loss collected in the drain during post-operative period was 310.89 ± 171.31ml in group TXA and 501.78± 135.83ml in group C (p=0.002) (Figure 1).
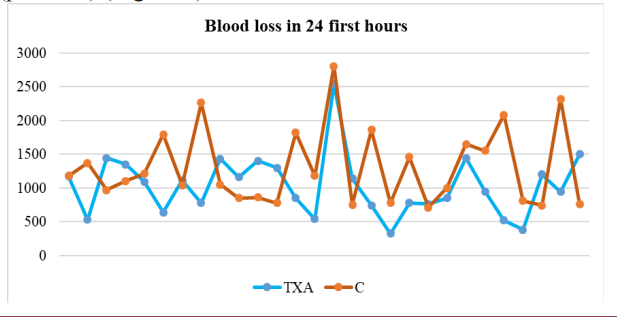
Figure 1: Blood loss during 24 first hours in the two groups.
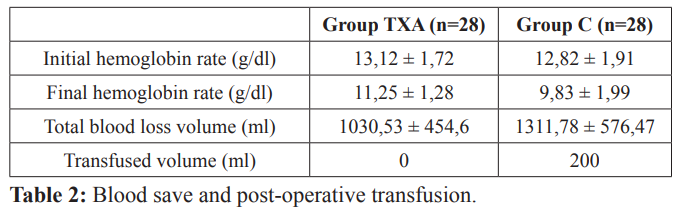
Total blood loss was estimated to 1030.53 ± 454.6ml for group TXA and 1311.78 ± 576.47ml for group C (p=0.045). The average hemoglobin rate in pre-operative was 13.12 ± 1.72g/dl in group TXA and 12.82 ± 1.91g/dl in group C (p=0.28). On day post- operative the average hemoglobin rate was quite higher in group TXA than in group C: 11.25 ± 128g/dl in group TXA versus 9.83± 1.99g/dl in group C. The difference between the initial and final hemoglobin rate was -1.87 ± 1.28g/dl in group ATX vs -2.99 ± 1.99g/dl in group C (p=0.009). On the first postoperative day, hemoglobin levels were higher in the TXA group: 11.25-1.28 g/ dl versus 9.83-1.99 g/dl (p=0.009). The difference between the initial and final hemoglobin rates was -1.87-1.28 g/dl in the TXA group and -2.99-1.99g/dl in the group control (p=0.009). Four (4) patients received blood transfusion in group C, no patient in the group TXA (p=0.11) (Table 2). All of our patients benefited from multimodal analgesia (paracetamol and tramadol) and a prevention of thromboembolic disease.
Discussion
During our study, 241 cases of femur fractures were operated in the trauma unit of Niamey National Hospital making a prevalence of 24.12%. Among those patients, 56 cases of femur fracture were included (23%). Our results are different from those of Abalo A et al. who reported a prevalence of 13.12% and an incidence of 3 cases for 10.000 persons [3]. This high number is explained by the occurrence of road injuries in our country [1,4,5]. Men were most concerned with sex ratio of 7. Several authors have also reported this male predominance [3,6,7]. Irisson E and al. found a parity between the two genders [8]. This male predominance can be explained by the fact that men are most highly exposed to public highway accidents because they represent the most important users of public roads and they have risky behavior [9]. The average age was 27.79 years in group TXA and 29.64 years in group C. Our result is similar to the Togo study which average age was 27 years [3]. It is inferior of Morocco study (68 years) [6]. This difference is linked to the fact that in our study patients who are more than 45 years old were not included. Also, studies about the efficacity of tranexamic acid in orthopedic and trauma surgery were more interested in osteosynthesis of proximal extremity of femur and protheses surgery of hip and knee which are most common in old persons. In our study road injuries trauma were the most common causes of femur fracture (94.64%), followed by ballistic injuries (3.57%) and domestic accidents with 1.79%. Abalo A et al. found a predominance of road injuries with 68.18% [3]. In our Serie, this high rate can be explained by the increase in vehicle fleets and the non-compliance of the highway code.
The average time for admission to operating room was 49.86 ± 76.74 days in group TXA versus 217.84 ± 365.20 days in group C. Morocco study found an average time of 12 days (4 and 21 days) from the trauma to surgery [6]. In Chad, authors reported an important average time of 83 ± 127 days (1 to 545 days). [10] Admission deadline is high in our context, this situation can be explained by the fact that patients first use traditional methods, a lack of technical platform, in addition to this the low socio- economic level of our patients and the lack of social security system.
About the thromboembolic prevention, enoxaparin was administered to 13patients (23.21%) in group TXA and 7patients (12.5%) in group C. Irison E et al. reported the administration of fondaparinux (27%) for TXA group versus 24% for control group, and administration of enoxaparinto73% in group TXA patients versus 76% in group C [8]. Anemia is common in anesthesia and Intensive Care Unit during peri-operative period. Our patients were not affected by anemia before surgery. Some authors found different results, especially a pre-operative anemia rate of 36% and 45% in trochanterian surgery [6,11]. There was no difference in per-operative blood loss between the two groups. Ours results are conform to the results of some authors [12-14] but different to some others [15-17]. However, there is a significant difference between the two groups about the volume of blood collected in Redon drains in our study which is conform to some other results [17].
Other studies have not found a significative difference between the two groups [6,18-19]. Our study confirms the effectiveness of tranexamic acid in reducing blood loss [1,8,20] and in improving post-operative hemoglobin rate [6,13,14,16]. Hemorrhagic surgery is associated with high blood transfusion rate, up to 70% in femur fracture surgery or hip prothesis revision, and 50% in total hip prothesis surgery [21]. Despite the use of different methods to lower per-operative bleeding, blood transfusion remains the essential condition to perform certain surgical procedures. Considerable progress in the field, blood transfusion is not without risks. That is why we should intensify searching of means that could allow us to reduce using [22]. The difference of blood transfusion use was significative in the two groups. The mean volume of packed red blood cells transfused in group C was 200ml versus 0ml in group TXA (p=0.002). In another study, there was no impact found in reducing blood transfusion by using tranexamic acid [20]. The randomized CRASH-2 study showed in trauma patients with bleeding risk that tranexamic acid allowed to reduce all causes of mortality from 16% to 14.5%, and to reduce hemorrhage mortality from 5.7% to 4.9% without increasing thrombotic accidents or acute renal injury cases [1].
Conclusion
Our study shows the efficacity of tranexamic acid for reducing blood loss in femur surgery, without increasing thrombotic complications, under reserve of respecting the contra indications. It’s an available product, with low cost and which safety had been proved in blood saving in femur surgery.
References
1.Zufferey PJ. Le point sur les antifibrinolytiques. Le Congrès Conférence d’Actualisation 2017. SFAR, Paris.16.
2.République du Niger Ministère des transports, Direction de la circulation et de la circulation sécurité routière annuaire statistique. 2012; 48.
3.Abalo A, Evegnon B, Ayouba G, et al. Epidémiologie et aspects anatomo-pathologiques des fractures du fémur à Lomé. Journal de la recherche scientifique de l’université de Lomé. 2009; 11.
4.Daddy H, Chaibou MS, James DL, et al. Prise en charge des accidents de la voie publique chez adultes admis aux urgences de l’Hôpital National de Niamey-Niger. RevAfrAnesth Med Urg. 2017; 22: 17-20.
5.DGPC, Direction Générale de la Protection Civile. Statistiques. 2017.
6.Bouchrit S. Intérêt de l’acide tranexamique dans le traitement des fractures trochantériennes par clou gamma standard. Thèse de médecine. Faculté de Médecine et de Pharmacie de Marrakech. 2018; 100.
7.Abdoul Wahab A.M, Koini M, Bembele B, et al. Anatomical and Functional Preliminary Results of Total Non Cemented HipProthese. Open Journal of Orthopedics. 2017; 7: 329-336.
8.Irisson E, Hemon Y, Pauly V, et al. L’acide tranexamique réduit les pertes sanguines et les coûts transfusionnels de la chirurgie prothétique de première intention. Revue de Chirurgie Orthopédique et Traumatologique. 2012; 98: 419- 425.
9.OMS, Organisation Mondiale de la Santé. Incidence mondiale. Rapport mondial sur la prévention des traumatismes dus aux accidents de la circulation. 2004; 2: 32-67.
10.Mathieu L, Mottier F, Bertani A, et al. Managment of neglected open extremity fractures in low-resource settings: Experience of the French army medical service in Chad. Orthopeadics and Traumatologie Surgery and Research. 2014; 100: 815-820.
11.Spahn DR. Anemia and patient blood management in hip and knee surgery: A systematic review of literature. Anesthesiology J. 2010; 113: 482-495.
12.Zufferey PJ, Miquet M, Quenet S, et al. Tranexamic acid in hip fracture surgery: a randomized controlled trial. BJA. 2010; 104: 23-30.
13.Fazilleau F, Clavé A, Dumser D, et al. Efficacité de l’acide tranexamique sur la déplétion sanguine dans les arthroplasties de hanche de première intention bénéficiant d’une anticoagulation par rivaroxaban. J RevChirurOrthoptraumatol. 2011; 97: 335-336.
14.Clavé A, Fazilleau F, Dumser D, et al. Efficacy of tranexamic acid on blood loss after primary cementless total hip replacement with rivaroxaban thromboprophylaxis: A case- control study in 70 patients. Orthopedics and Traumatology Surgery and Research. 2012; 98: 484-490.
15.Bhatia SK, Deshpande H. Rôle de l’acide tranexamique dans la réduction de la perte de sang pendant et après la césarienne. Med YDY Patil Univ. 2015; 8: 25-35.
16.Karimi A, Mohammadi SS, Hasheminasab M, et al. Efficacy of
tranexamic acid on blood loss during bimaxilary osteotomy: a randomized double-blind clinical trial. Saudi J Anesth. 2012; 6: 41-45.
17.Ekback G, Axelsson K, Ryttberg L, et al. Efficacy of tranexamic acid reduces blood loss in total hip replacement surgery. Anesth Anal. 2000; 91: 1124-1130.
18.Jinlei L, Binfei Z, Cong Y, et al. Tranexamic acid reduces hidden blood loss in the treatment of intertrochanteric fractures with PFNA: a single center randomized controlled trial. Journal of Orthopedic Surgery and Research. 2017; 12: 124.
19.Virani S, Panda I, Dahapute A, et al. Role of local infiltration of tranexamic acid in reducing blood loss in peritrochanteric fracture surgery in elderly population. MalaysOrthop J. 2016; 10: 26-30.
20.Ribette E, A.-L. Saint-pol, Fescau C, et al. Epargne sanguine, apport de l’acide tranexamique dans la chirurgie du rachis. Annfar. 2013; 32: 142-143.
21.Bonhomme F. Le saignement au bloc opératoire. Le Congrès Médecins. Conférence d’essentiel. SFAR 2014.
22.SFAR, Société Française d’Anesthésie Réanimation. Les apports d’érythrocytes pour la compensation des pertes sanguines en chirurgie de l’adulte. Conférence de consensus ANDEM. Paris 1993.