The Neurobiology of Addiction
Author'(s):Julian Ungar-Sargon*
Franciscan Hospital System, Rensselaer, IN 47978.
*Correspondence:
Julian Ungar-Sargon, MD PhD, Franciscan Hospital System, E-mail: Jyungar@mac.com, www.jyungar.com.
Received: 24 Mar 2024; Accepted: 28 Apr 2024; Published: 04 May 2024
Citation: Ungar-Sargon J. The Neurobiology of Addiction. Addict Res. 2024; 8(1): 1-7.
Keywords
Definitions
Substance-use disorder: A diagnostic term in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM- 5) referring to recurrent use of alcohol or other drugs that causes clinically and functionally significant impairment, such as health problems, disability, and failure to meet major responsibilities at work, school, or home. Depending on the level of severity, this disorder is classified as mild, moderate, or severe.
Addiction: A term used to indicate the most severe, chronic stage of substance-use disorder, in which there is a substantial loss of self-control, as indicated by compulsive drug taking despite the desire to stop taking the drug. In the DSM-5, the term addiction is synonymous with the classification of severe substance-use disorder.
Addiction is a disease characterized by behavioral issues, and dependence refers to a physical reliance on a substance. The two conditions often occur at the same time, but a person can be dependent on a substance without being addicted to it. Addiction is synonymous with substance use disorder, and abuse means the same thing as misuse.
A person with an addiction uses a substance, or engages in a behavior, for which the rewarding effects provide a compelling incentive to repeat the activity, despite detrimental consequences. Addiction may involve the use of substances such as alcohol, inhalants, opioids, cocaine, and nicotine, or behaviors such as gambling or pornorgraphy.
There is evidence that addictive behaviors share key neurobiological features: They intensely involve brain pathways of reward and reinforcement, which involve the neurotransmitter dopamine.
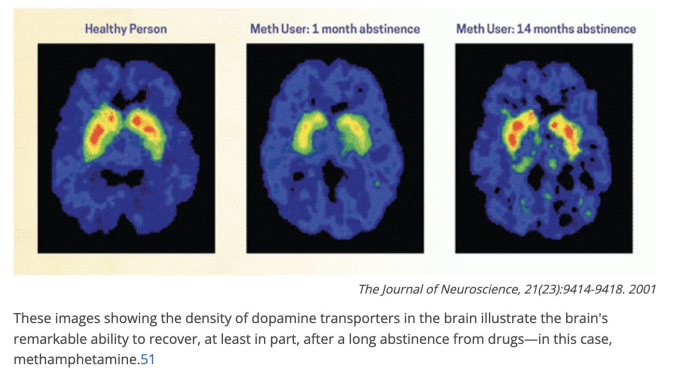
nd, in keeping with other highly motivated states, they lead to the pruning of synapses in the prefrontal cortex, home of the brain's highest functions, so that attention is highly focused on cues related to the target substance or activity. It is important to know that such brain changes are reversible after the substance use or behavior is discontinued.
Chemical/Brain model
In the past decades, research has increasingly supported the view that addiction is a disease of the brain. Although the brain disease model of addiction has yielded effective preventive measures, treatment interventions, and public health policies to address substance-use disorders, the underlying concept of substance abuse as a brain disease continues to be questioned, perhaps because the aberrant, impulsive, and compulsive behaviors that are characteristic of addiction have not been clearly tied to neurobiology.
In the United States, 8 to 10% of people 12 years of age or older, or 20 to 22 million people, are addicted to alcohol or other drugs. The abuse of tobacco, alcohol, and illicit drugs in the United States exacts more than $700 billion annually in costs related to crime, lost work productivity, and health care.
After centuries of efforts to reduce addiction and its related costs by punishing addictive behaviors failed to produce adequate results, recent basic and clinical research has provided clear evidence that addiction might be better considered and treated as an acquired disease of the brain.
Research guided by the brain disease model of addiction has led to the development of more effective methods of prevention and treatment and to more informed public health policies.
Nonetheless, despite the scientific evidence and the resulting advances in treatment and changes in policy, the concept of addiction as a disease of the brain is still being questioned. The concept of addiction as a disease of the brain challenges
deeply ingrained values about self-determination and personal responsibility that frame drug use as a voluntary, hedonistic act. In this view, addiction results from the repetition of voluntary behaviors. How, then, can it be the result of a disease process?
Stages of Addiction
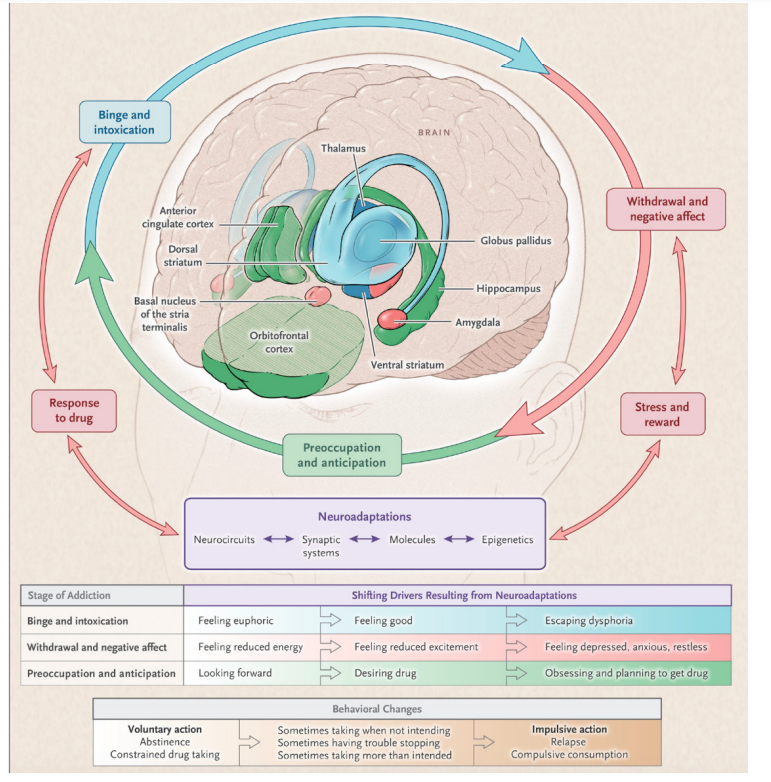
We have divided addiction into three recurring stages: binge and intoxication, withdrawal and negative affect, and preoccupation and anticipation (or craving).10 Each stage is associated with the activation of specific neurobiologic circuits and the consequential clinical and behavioral characteristics.
Stages of the Addiction Cycle
During intoxication, drug-induced activation of the brain’s reward regions (in blue) is enhanced by conditioned cues in areas of increased sensitization (in green). During withdrawal, the activation of brain regions involved in emotions (in pink) results in negative mood and enhanced sensitivity to stress. During preoccupation, the decreased function of the prefrontal cortex leads to an inability to balance the strong desire for the drug with the will to abstain, which triggers relapse and reinitiates the cycle of addiction. The compromised neurocircuitry reflects the disruption of the dopamine and glutamate systems and the stress-control systems of the brain, which are affected by corticotropin-releasing factor and dynorphin. The behaviors during the three stages of addiction change as a person transition from drug experimentation to addiction as a function of the progressive neuroadaptations that occur in the brain [1].
Neuroadaptations to Chronic Substance Exposure Tolerance
As a drug is consumed regularly, a higher dose may be required to achieve a response equivalent to that experienced following initial consumption. This is termed tolerance and results from neuroadaptive changes in the brain to maintain homeostasis. Owing to the wide range of pharmacological mechanisms of different drugs of misuse, such neuroadaptations may vary dependent on both the drug and the individual. It is also important to note that tolerance to behavioural and physiological effects of drugs may develop at different rates.
Withdrawal
Following these neuroadaptations, abrupt cessation of the drug leaves the brain unable to achieve homeostasis, resulting in withdrawal characterised by dysphoria, emotional stress, and a decrease in cognitive ability. Just as neuroadaptive changes differ for each drug of misuse and individual, so do some withdrawal symptoms. Some drugs, such as alcohol and opiates, produce significant physiological withdrawal symptoms (e.g., alcohol: tremors, sweating, nausea, seizures, etc.; opiates: muscle aches, lacrimation, sweating, diarrhoea), whereas others more prominently cause emotional symptoms (e.g., stimulants: depression). Withdrawal often perpetuates drug use or leads to relapse as an individual attempts to overcome its negative effects. As the brain adapts to the absence of the drug, generally withdrawal diminishes over days to weeks.
Relapse
For those individuals who achieve abstinence, risk of relapse remains high and although this risk is reduced over time it never completely disappears. Relapse may occur years after achieving abstinence, in response to environmental stressors, low mood or stress during the preoccupation/anticipation phase of the substance dependence associated with enduring dysregulation in key brain processes such as reward and inhibitory control.
Binge and Intoxication
All known addictive drugs activate reward regions in the brain by causing sharp increases in the release of dopamine. At the receptor level, these increases elicit a reward signal that triggers associative learning or conditioning. In this type of Pavlovian learning, repeated experiences of reward become associated with the environmental stimuli that precede them. With repeated exposure to the same reward, dopamine cells stop firing in response to the reward itself and instead fire in an anticipatory response to the conditioned stimuli (referred to as “cues”) that in a sense predict the delivery of the reward. This process involves the same molecular mechanisms that strengthen synaptic connections during learning and memory formation.
Withdrawal and Negative Affect
An important result of the conditioned physiologic processes involved in drug addiction is that ordinary, healthful rewards lose their former motivational power. In a person with addiction, the reward and motivational systems become reoriented through conditioning to focus on the more potent release of dopamine produced by the drug and its cues. The landscape of the person with addiction becomes restricted to one of cues and triggers for drug use. However, this is only one of the ways in which addiction changes motivation and behavior.
Addiction is a global health problem with a chronic relapsing nature for which there are few treatment options. In the past few decades, neuroimaging has allowed us to better understand the neurobiology of addiction. Functional neuroimaging paradigms have been developed to probe the neural circuits underlying addiction, including reward, inhibitory control, stress, emotional processing, and learning/memory networks.
Criticisms
As with all medical advances, science is provisional and humble, always bowing to the next better clinical study or trial. Looking objectively at statistics using evidenced based medical critical analysis reveals that in addiction treatments the data is not all clear.
Overlaps in brain abnormalities between people with addiction and control groups, raises questions on the role that brain abnormalities have on addiction.
The overlap is likely to reflect the limitation of currently available brain imaging techniques (spatial and temporal resolutions, chemical sensitivity), our limited understanding of how the human brain works, the complexity of the neurobiological changes triggered by drugs and the heterogeneity of substance use disorders [2].
Treatment benefits associated with the Brain Disease Model of Addiction have not materialized.
Medications are among the most effective interventions for substance use disorders for which they are available (nicotine, alcohol, and opiates). Moreover, progress in the approval of new medications for substance use disorders has been slowed by the reluctance of pharmaceutical companies to invest in drug development for addiction [3].
How do behavioral therapies treat drug addiction? Behavioral addictions
The concept of behavioral addictions has been controversial particularly as it relates to the concept of “food addiction” and its contribution to obesity [4]. However, there is increasing recognition that the rewarding effects of food, particularly food rich in fat and sugar, can trigger neuroadaptations in the brain reward and stress circuitry that are similar to those produced by addictive drugs [5]. Interestingly, peripheral signals involved in satiety and hunger (i.e., leptin, insulin, ghrelin) that influence the sensitivity of the brain dopamine system to the rewarding effects of food also modulate the sensitivity to the rewarding effects of various drugs [6]. Studies have also identified significant overlaps (though also unique differences) among the brain circuits affected in addiction and obesity [7]. Similarly, it is interesting that cues repeatedly associated with fat/sugar rich foods (e.g., TV commercials) also appear to acquire the power to produce exaggerated reactivity (craving) and reduced control over food intake; as well as increased negative emotional reactivity when attempting to refrain from eating [8]. Pharmacological studies have also shown that medications used in the treatment of addiction (naltrexone/bupropion) can be beneficial for the treatment of obesity [9] and medications for obesity may hold promise for addictions (lorcaserin) [10]. Similarly, behavioral interventions beneficial in the treatment of addiction have shown benefit in the treatment of obesity [12]. The current consensus is that only a subset of individuals with obesity (those with a binge-eating disorder) suffers from “food addiction”. However, the DSM-5, does not include binge-eating disorder among the addictive disorders. Internet gaming is the only non- substance based disorder considered by DSM-5 as an addictive disorder.
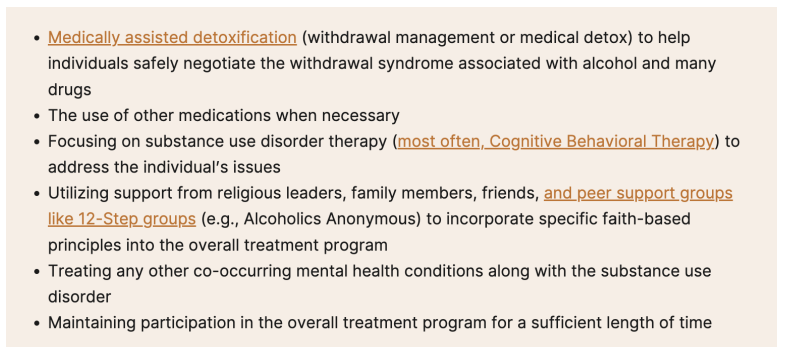
Behavioral therapies help people in drug addiction treatment modify their attitudes and behaviors related to drug use. As a result, patients are able to handle stressful situations and various triggers that might cause another relapse. Behavioral therapies can also enhance the effectiveness of medications and help people remain in treatment longer.
Cognitive-behavioral therapy seeks to help patients recognize, avoid, and cope with the situations in which they're most likely to use drugs.
Contingency management uses positive reinforcement such as providing rewards or privileges for remaining drugfree, for attending and participating in counseling sessions, or for taking treatment medications as prescribed.
Motivational enhancement therapy uses strategies to make the most of people's readiness to change their behavior and enter treatment.
Family therapy helps people (especially young people) with drug use problems, as well as their families, address influences on drug use patterns and improve overall family functioning.
Twelve-step facilitation (TSF) is an individual therapy typically delivered in 12 weekly sessions to prepare people to become engaged in 12-step mutual support programs. 12- step programs, like Alcoholic Anonymous, are not medical treatments, but provide social and complementary support to those treatments. TSF follows the 12-step themes of acceptance, surrender, and active involvement in recovery.
Recovery
Does alcoholics anonymous involvement predict treatement outcome
Patients receiving inpatient treatment for alcohol dependence were followed for 31 weeks after discharge. Alcoholics Anonymous (AA) attenders, when compared with nonattenders, were not distinguishable on pretreatment patient characteristics. Posttreatment attendance of AA was not predictive of drinking outcomes. However, a measure of the degree to which patients had become involved in AA did predict more favorable outcomes [12].
Alcoholics Anonymous, the worldwide fellowship of sobriety seekers, is the most effective path to abstinence, according to a comprehensive analysis conducted by a Stanford School of Medicine researcher and his collaborators.
AA began in 1935 when two men in Akron, Ohio, were searching for a way to stay sober; they found it by forming a support group. They later developed the 12 steps, the first being accepting one’s inability to control drinking; the last, helping others sustain sobriety by becoming a sponsor of a new member. The AA model- open to all and free - has spread around the globe, and AA now boasts over 2 million members in 180 nations and more than 118,000 groups. Though the fellowship has been around for more than eight decades, researchers have only recently developed good methods to measure its effectiveness, Humphreys said. Most of the studies that measured abstinence found AA was significantly better than other interventions or no intervention. In one study, it was found to be 60% more effective. None of the studies found AA to be less effective [13].
The Instincts [14]
What makes sexual, food and gambling recovery so hard? Why do those addictions have such low recovery rates? Substance addiction involves the misuse of instincts, addictions involving food, sex or money are addiction to instinctive behaviour.
What makes sexual, food and gambling recovery so hard? Why do those addictions have such low recovery rates? Substance addiction involves the misuse of instincts, addictions involving food, sex or money are addiction to instinctive behaviour.
CREATION gave us instincts for a purpose. Without them we wouldn’t be complete human beings….(instinctive) desires… are perfectly necessary and right, and surely God-given. Yet these instincts, so necessary for our existence, often far exceed their proper functions. Powerfully, blindly, many times subtly, they drive us, dominate us, and insist upon ruling our lives…. When thus out of joint, man’s natural desires cause him great trouble, practically all the trouble there is. No human being, however good, is exempt from these troubles. Nearly every serious emotional problem can be seen as a case of misdirected instinct. When that happens, our great natural assets, the instincts, have turned into physical and mental liabilities [15].
When the addiction is to instinctive behaviour, more complex thinking is required to manage triggers than with drugs, alcohol, or smoking, where the standard recovery mantra is “stay out of the old environment and don’t pick up the first drink, drug or cigarette.”
The survival instincts for food, sex and finances are built into the brain and are largely automatic. The body and brain is the old environment, not some external place we visit to procure our drug of choice. Recovery from addiction to instinctive behaviour requires managing instinctive urges at a high level. This requires a sufficiently functioning brain and in particular, a well enough functioning neocortex (thinking brain) to overpower the impulses from the automatic survival (reptilian) brain.
Hassidism and Recovery
The revolutionary movement within Judaism in 18th century Eastern Europe, like its counterparts in Christianity, centered upon a deep concern with inner spirituality. Most importantly was the Hassidic Master, Rabbi Nachman of Bratzlav (Ukraine) whose devotions included meditation, prayer and deep inner reflection (Hitbodedut). He was also concerned with addictive behavior, so that, for instance, alcohol was not permitted in gatherings of his hassidim and a focus on sexual purity (Tikkun HaBris) was a prerequisite for any mystical contact with the divine.
Rabbeinu and Addiction
In Breslov there’s an emphasis on personal development and a refreshing de-emphasis on many types of group-imposed external manifestations of piety. Also, because the Rebbe didn’t shy away from boldly addressing popular modern topics, from sex and drugs to music and food, navigating familial and societal pressures, depression and anxiety, meditation, and prayer, and of course, spirituality, birth, and death, Breslov is often cited as the body of Hasidic thought most essential to our times.
Others have discussed a rabbinic approach to addiction like Rabbi Joey Rozenfeld: [16]
1. When speaking of “addiction”, we are not referring to the diagnostic category of substance abuse related diseases or addiction as a mental illness. To attempt to speak of the spiritual world of the lived experience of addiction as a disease would be grossly inappropriate. This is not to say that there is no spiritual dimension to the experience of addiction, but rather that focusing on the spiritual and abstract expression of this condition while the individual is in the midst of real suffering is unethical in the truest sense. Addiction is a destructive disease that makes life nearly unlivable for the addict and anyone who loves the addict. The symptoms of addiction often result in abject suffering and death and as such any attempt to relegate this disease to the realm of spirituality is to ignore the significant role that both the brain and the body play in this disease and its treatment.
2. For Rabbeinu, the word and concept of “addiction” can be used in the most expansive form so as to include any mode of inner experience that drives the individual towards escaping life. Addiction is never simply addiction to a drug or chemical, but rather it is always already the sum total of suffering, despair, and an attempted response to pain. While this pain may often be physical and neurobiological in nature, for the purpose of these classes we will be examining the psycho-spiritual pain that the individual experiences within the self/soul as opposed to the brain/body. In this sense any inner experience that results in the individuals attempt to escape life will be considered to be part and parcel of the addiction experience.
3. When speaking of addiction, we are not simply referring to the maladaptive attachment to mind altering chemicals such as alcohol or drugs. When addiction is limited to the space of mind altering chemicals a sharp distinction is made between us and them. “Us” as the normal, functioning individuals who have not undergone the process of physical tolerance and dependency, and “them” as the individuals who have gone through the process of use, misuse and abuse developing a tolerance and dependency on mind altering chemicals. In order to insure that we move away from the misleading platitudes that have littered the field of addiction wherein one is either addicted or not addicted; we would like to posit that everybody qua human being lives within the possibility-of- addiction. Whether process addictions in the form of repetitive behaviors that ease the everyday pains of life, or the insistence of negative habits and traits, addiction is something that affects each and every person whether or not they have moved from the realm of potential possibility into the realm of actual experience.
4. The guiding principle is that addiction is rooted within the recesses of the soul and as such the soul is the place where comfort and recovery must come from. The soul of the addict or the addicted soul is one that contains within itself vast storehouses of intensity and desire. It is for this reason that the process out of addiction towards recovery offers gifts that could never have been realized without addiction. In this sense, addiction will be seen as a profoundly difficult condition that can give birth to an equally if not more profound sense of spiritual sensitivity and experience. One need not have experienced the descent into addiction in order to benefit from the ascent out of it; one must simply be willing to pay mind to the possibility-of-addiction that abides within each individual qua human being.
Nowhere more than is the area of Tikkun Habris does Rabbeinu address the deepest damage to the human soul. Here the specific “S fellowships” operate in approaching the management of powerlessness over lust especially pornography.
Many of us came to Sexaholics Anonymous (SA) driven to total despair by our destructive sexual thoughts and behaviors. Within the meeting rooms of SA we discovered, to our surprise, that lust was the driving force behind our acting out. Sexual lust is an inordinate thought or feeling that drives us to use ourselves, others, or things for self-centered destructive purposes. The spiritual sickness of lust wants sexual stimulation at that moment instead of what a Higher Power or God of our understanding is offering us. Later we come to see that lust wants anything other than what has offered us each moment. At first it was hard to believe. As we began to accept this fact, we wondered how we could live without lust. It became clear that we had to give it up, yet we doubted that life without lust was possible [17].
It is here that Breslov chassidus becomes synchronous with the 12 step recovery program most.
For Rabbeinu, the tools of recovery center around physical, mental, and spiritual rectification:
Mikveh/Tikkun Klali and Hitbodedut. In the words of Rebbe Natan:
Be very careful to immerse in a mikveh (ritual pool) on the same day that you have an unclean experience. It is best to immerse immediately, but if you are unable to immerse first thing in the morning, do so at any time during the day, even towards evening. It is very important to immerse on the same day.
Everyone experiences a chance emission at some time or other. I call you to bear witness that these Ten Psalms are a very effective remedy: they are the complete remedy.
Others experience emissions because of their bad thoughts. This literally creates impure forces. But even in such cases recital of the Ten Psalms will do much to remedy the spiritual damage.
The remedy of the Ten Psalms is entirely original. It is a most wonderful and awesome remedy.
It is certainly best if you can immerse in a mikveh and then say the Ten Psalms. But even if you are sick or traveling and unable to immerse, reciting the Psalms alone is a great remedy. If you can say the Psalms with devotion and feeling, it is best. But even just saying the words helps.
This remedy has not been revealed since the time of creation [18].
Rebbe Nachman's main teaching on Tikkun HaKlali was given on Shavuot 5566 (May 23, 1806). Yet he did not reveal the specific ten Psalms of the Tikkun HaKlali until April 1810. At that time, Rebbe Nachman revealed the specific ten Psalms [19] to two of his closest disciples, Rabbi Aharon of Breslov and Rabbi Naftali of Nemirov, making them witnesses for an unprecedented vow:
One of the principal spiritual practices that Rabbi Nachman taught was hitbodedut, praying to God in one’s own words and native language about personal hopes, trials, and dreams. If possible, hitbodedut should be done in a wilderness area at night, to achieve complete isolation, but it can be performed anywhere, even under a blanket. He taught that hitbodedut should ideally be practiced for one hour each day and if a Jew persists in practising it, he/she will learn to experience God’s closeness, and to see the hidden light that illuminates all of existence.
The 12 steps of AA upon which Roy K. based his writings and experience for SA, centers around similar concepts and spiritual practices. If lust is a false connection or substitute with another, then surrender to a higher power and rectifying one’s character defects are the way back to a real connection with Hashem and other human beings [20].
References
1. Nora D Volkow, A Thomas McLellan, George F Koob. Neurobiologic Advances from the Brain Disease Model of Addiction. N Engl J Med. 2016; 374: 363-371.
2. Hall W, Carter A, Forlini C. The brain disease model of addiction is it supported by the evidence and has it delivered on its promises. Lancet Psychiatry. 2015; 2: 105-110.
3. Higgins ST, Sarah H Heil, Stacey C Sigmon. Voucher-based contingency management in the treatment of substance use disorders. APA Psycnet. 2013; 2: 481-500.
4. McLellan AT, Woodworth AM. The affordable care act and treatment for substance use disorders implications of ending segregated behavioral healthcare. J Subst Abuse Treat. 2014; 46: 541-545.
5. DeFulio A, Everly JJ, Leoutsakos JM, et al. Employment-based reinforcement of adherence to an FDA approved extended release formulation of naltrexone in opioid-dependent adults a randomized controlled trial. Drug Alcohol Depend. 2012; 120: 48-54.
6. Manolio TA, Collins FS, Cox NJ, et al. Finding the missing heritability of complex diseases. Nature. 2009; 461: 747-753.
7. Bevilacqua L, Goldman D. Genes and addictions. Clin Pharmacol Ther. 2009; 85: 359-361.
8. Busch SH, Epstein AJ, Harhay MO, et al. The effects of federal parity on substance use disorder. Am J Manag Care. 2014; 20: 76-82.
9. Salamone JD, Correa M. Dopamine and food addiction lexicon badly needed. Biol Psychiatry. 2013; 73: e15-e24.
10. Volkow ND, Wang GJ, Tomasi D, et al. The addictive dimensionality of obesity. Biol Psychiatry. 2013; 73: 811-818.
11. Egecioglu E, Skibicka KP, Hansson C, et al. Hedonic and incentive signals for body weight control. Rev Endocr Metab Disord. 2011; 12: 141-151.
12. Tomasi D, Volkow ND. Striatocortical pathway dysfunction in addiction and obesity differences and similarities. Crit Rev Biochem Mol Biol. 2013; 48: 1-19.
13. Cottone P, Sabino V, Roberto M, et al. CRF system recruitment mediates dark side of compulsive eating. Proc Natl Acad Sci U S A. 2009; 106: 20016-20020.
14. Butsch WS. Obesity medications: what does the future look like. Curr Opin Endocrinol Diabetes Obes. 2015; 22: 360-366.
15. Higgins GA, Fletcher PJ. Therapeutic Potential of 5-HT2C Receptor Agonists for Addictive Disorders. ACS Chem Neurosci. 2015; 6: 1071-1088.
16. Volkow ND, O'Brien CP. Issues for DSM-V: should obesity be included as a brain disorder. Am J Psychiatry. 2007; 164: 708-710.
17. Henry A Montgomery, William R Miller, J Scott Tonigan. Does alcoholics anonymous involvement predict treatment outcome. Journal of Substance Abuse Treatment. 1995; 12: 241-246.
18. Mandy Erickson: https://med.stanford.edu/news/all-news/2020/03/alcoholics-anonymous-most-effective-path-to-alcohol-abstinence.html
19. https://www.joeyrosenfeld.com/residualspeech/2019/1/30/the-inner-world-of-addiction