The Use of Musculoskeletal Ultrasound to Demonstrate the Reflection Pulley of the Shoulder
Author'(s): Michael Meng, DC, RMSK*
San Diego Pain Consultants, 15725 Pomerado Rd #105 Poway, US.
*Correspondence:
Michael Meng D.C. RMSK, San Diego Pain Consultants, 15725 Pomerado Rd #105 Poway, CA 92064, US, Tel: 619-254-0409;E-mail: mikejmeng@gmail.com.
Received: 14 March 2018; Accepted: 08 April 2018
Citation: Akiko Ando, Takeshi Umegaki, So Yamaki, et al. Thoracic Endovascular Aortic Repair in a Patient with Dilated Cardiomyopathy and Low Ejection Fraction: A Case Report. Anesth Pain Res. 2018; 2(1): 1-4.
Abstract
Musculoskeletal ultrasound, static and dynamic imaging can be a useful modality to assess the rotator cuff interval, A clinical significant anatomic region of the shoulder. Due to anatomic location the rotator cuff interval is difficult to assess via MRI imaging, clinical testing and even through arthroscopic techniques. Without radiation, equipment accessibility, low cost, and low patient burden Ultrasound should be considered in anterior shoulder pain patients.
Keywords
Introduction
The reflection pulley is a ligamento-capsulotendinous sling complex that provides stability to both the long head of the biceps tendon and glenohumeral joint. The pulley is subject to a variety of pathologic conditions as a result of trauma, degenerative, and inflammatory changes. As part of the rotator cuff interval, the reflection pulley is subject to a number of important surgical considerations. Furthermore, since the reflection pulley is intimately involved with the long head of the biceps tendon which is highly innervated with nociceptive fibers, the pulley and associated biceps tendon can serve as a nidus for shoulder pain. Pathologic lesions of the biceps pulley mechanism are notoriously difficult to identify on physical examination and magnetic resonance imaging (MRI) and have thus been called the “hidden lesions” of the shoulder [1,2].
The reflection pulley and its individual contributory components are difficult to visualize with MRI, although MR arthrography can provide important anatomic and clinical information as can both static and dynamic [3].
Anatomic Considerations
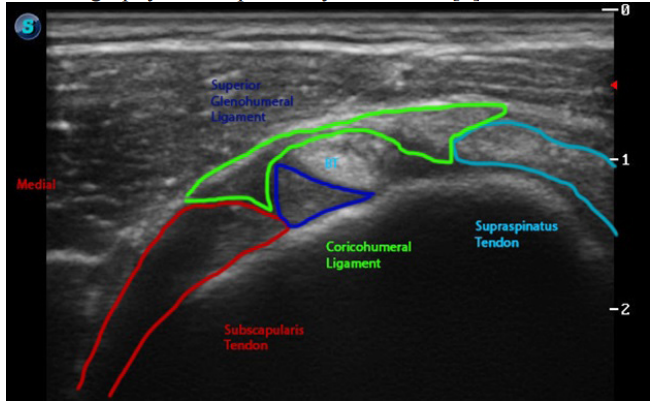
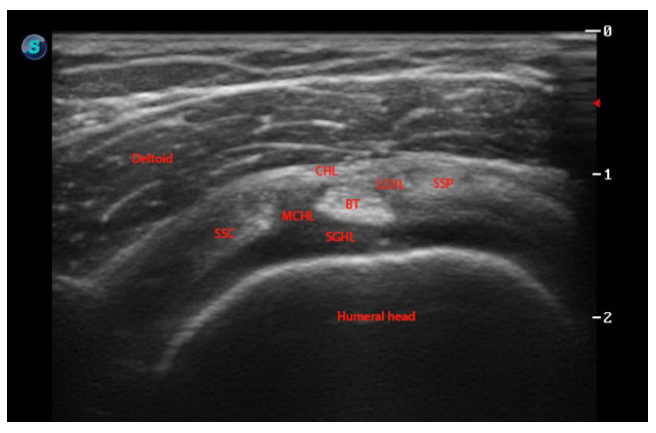
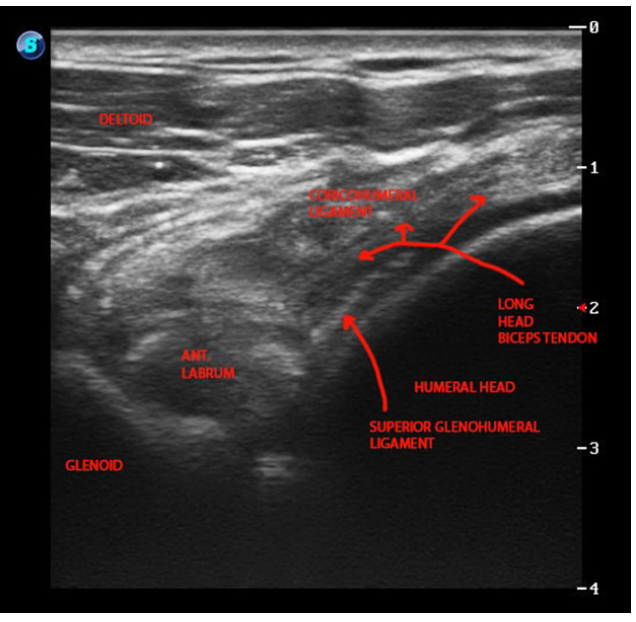
The reflection pulley is located within the rotator cuff inteval and is formed by fibers from the supraspinatus tendon, subscapularis tendon, coracohumeral ligament, and super glenohumeral ligament. The coracohumeral ligament arises from the lateral coracoid base (proximal third of the dorsolateral aspect) and divides into two major bands known as the medial and lateral bundle. The medial bundle of the coracohumeral ligament crosses the rotator cuff interval, and is bounded on its medial and inferior aspects by the long head of the biceps tendon. The medial bundle inserts on the lesser tuberosity of the humerus along with the superior fibers of the subscapularis tendon (Figure 1) [3]. The lateral bundle of the coracohumeral ligament abuts the superior and lateral portion of the long head of the biceps tendon to insert on the greater tuberosity along with fibers from the supraspinatus tendon. The medial bundle fibers blend with fibers from the subscapularis tendon and the superior glenohumeral ligament to form the medial-pulley complex (Figure 1). In a similar fashion, the contribution of fibers from the lateral coracohumeral bundle, supraspinatus tendon, and superior glenohumeral ligament form the lateral-pulley complex. While in the reflection pulley the biceps tendon is intracapsular but extrasynovial (Figures 1-4) [3,4].
The richly innervated proximal portion of the long head of the biceps tendon curves 30-45 degrees within the reflection pulley before entering the bony intertubercular groove. This curvature subjects this portion of the biceps tendon to significant torsionalstrain. Additional strain on the tendon occurs as the biceps passes beneath the transverse humeral ligament and into the bicipital groove. The reflection pulley’s main function is to protect the long head of the biceps tendon from translational forces to the shoulder and impingement as it passes beneath the coracohumeral arch.
The coracohumeral ligament and its medial and lateral bundles are clearly demonstrated with static ultrasound imaging (Figures 1-4) [4]. The anterior bundle of the coracohumeral ligament limits extension, inferior and posterior translation of the humeral head, and serves as the ceiling for the long head of the biceps in this segment. The posterior bundle of the coracohumeral ligament limits flexion, inferior and posterior translation of the humeral head [5]. Armed with this functional anatomic knowledge, the ultrasongraphy can utilize static and dynamic ultrasonography to identify pathologic lesions of both the anterior and posterior bundles (Figures 1-4). Patient placed in stress position for assessment of the ligament - modified crass with posterior translation. The thickness of the coracohumeral ligament at the reflection pulley can also be measured with ultrasound. Preliminary studies suggest that thickening of the coracohumeral ligament at the reflection pulley is often seen in arthroscopically confirmed cases of adhesive capsultitis, with the average thickness of the ligament in non- painful control shoulders of 1.34 to 1.39 mm [6].
The superior glenohumeral ligament acts as the floor of the reflection pulley, running from the anterior labrum at the superior glenoid tubercle to the lesser tuberosity. The ligament forms a U shaped sling that cradles the long head of the biceps tendon and functionally protects the proximal biceps tendon from sheering forces at the proximal bicipital groove [7,8]. It has been hypothesized that the stability of the long head of the biceps tendon may plays contribute to anterior labrum tears, in particular with SLAP lesions where the biceps anchor is intact and there is a labral tear. It is believed the increased torsion placed on the labrum by the long head of the biceps tendon resulting in a peel-back mechanism that occurs during the cocking phase of the throwing motion at the superior labrum anchor (Figures 1-4) [9].
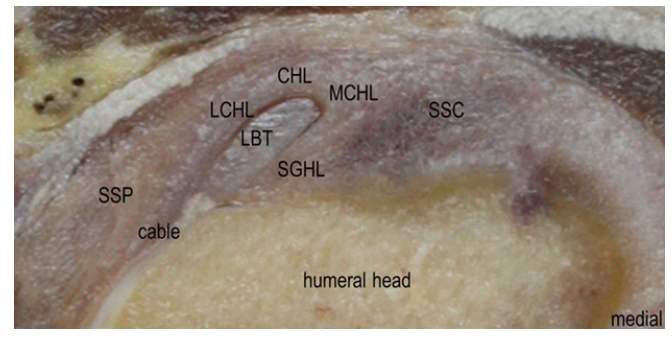
Medial to the long head of the biceps tendon at the reflection pulley is the subscapularis tendon. Lateral to the long head of the biceps tendon is supraspinatus tendon, thus completing the margins of the reflection pulley. Distal to the reflection pulley fibers, the fibers of the respective tendons form the transverse humeral ligament at the bicipital groove. Tearing of the subscapularis is difficult to diagnosis; however, resisted internal rotation under dynamic ultrasonography can help identify these tears [1].
Ultrasonographic Considerations
MR arthography is the most sensitive imaging modality available to identify pathologic lesions of the reflection pulley and non- invasive static and dynamic ultrasonography can also identify many lesions of the reflection pulley. Chung at al. reported that MRI was only able to identify the corocohumeral ligament component of the reflection pulley in 60% of cases [10].
Specific pathologic conditions that can be assessed by MR arthrography and ultrasonography include: anterosuperior impingement, instability of the biceps tendon, biceps tendinopathy, biceps entrapment, biceps subluxation, split biceps, tenosynovitis, tendinosis, anterior and posterior lesions of the superior labrum, adhesive capsulitis, subscapularis impingement, superior glenohumeral ligamentous injury, and coracohumeral ligament injury can be evaluated at the reflection pulley. These lesions may be caused by inflammation, degenerative changes, instability, and impingement,
Inflammatory
The synovial lining of the biceps tendon sheath is continuous with the glenohumeral joint, thus intimately related to conditions occurring in the joint such as impingement and rotator cuff tendinopathy. Biceps tenosynovitis can also be observed [11]. The appearance of synovitis, pannus, and or hyperemia may be readily apparent with color power Doppler scanning.
Degenerative
Translational forces, and laxity, ligament thinning / thickening may be visible on ultrasound examination being an anterior structure. The long head of the biceps tendon is subject to impingement at the coricoacomial arch. Overhead activities such as pitching and overhead work may exacerbate the pathologic process. Further anterior laxity of the glenohumeral joint can contribute to sheering of the long head of the biceps tendon at the rotator cuff, specifically at the superior glenohumeral ligament - sling mechanism [12-14].
Depiction of adhesive capsulitis is often illustrated by thickening of the coricohumeral ligament. Thickness of the coracohumeral ligament at the reflection pulley can readily measure with ultrasound as mentioned above. Preliminary studies demonstrate that the maximum thickness of the coricohumeral ligament to be increased to 3 mm in arthroscopically confirmed cases of adhesive capsulitis over painful and non-painful shoulders with average thickness of 1.34 to 1.39 mm respectively [6].
Instability
Biceps tendon subluxation and dislocations are readily apparent with ultrasonographic examination. Typically the tendon will sublux medially toward the subscapaularis tendon. This motion is well depicted with dynamic ultrasound examination with abduction and external rotation of the affected shoulder [15,16].
Impingement
Subscapularis impingement syndrome and other “hidden,” rotator cuff interval lesions have been described. Ultrasound may provide a useful modality for detection due to the ability to dynamically test for these conditions. In a study of 165 patients treated arthroscopically for anterior instability and rotator cuff syndromes, WF Bennet, noted that the incidence rate of subscapularis tendon involvement was 27%. The incidence rate of subscapularis tendon disruptions with rotator cuff pathology was 35%. The incidence rate of superior glenohumeral ligament was 18%. The incidence rate of superior glenohumeral ligament tears was 15%. Forty- seven percent of all subscapularis tears involved the rotor cuff interval complex [17-20].
SLAP lesions
Due to the origin of the long head of the biceps tendon on the anterior labrum and the commonality of the long head of the biceps through the supporting reflection pulley as well as the commonality in mechanism of injury, it is reasonable the injury to one site is suggestive of injury to the other. Ultrasonic evaluation may provide a limited, but important role in the identification of hidden lesions of the shoulder for instability, inflammatory changes, impingement, and biceps tendon pathologies and should be considered in the initial evaluation of these lesions before moving on to MR arthography.
The rotator cuff interval of the shoulder is a clinically important region. The significance of the structures if often overlooked and under-appreciated in clinical practice. Many painful conditions can manifest in in the rotator cuff interval; and with proper detection, better treatment outcomes may be possible.
References
1.Ryan J. Krupp, Mark A. Kevern, Michael D. Gaines, et al. Long Head of the Biceps Tendon Pain: Differential Diagnosis and Treatment. J Orthop Sports Phys Ther. 2009; 39: 55-70.
2.Altchek D, Wolf B. Disorders of the biceps tendon. In: Krishnan S, Hawkins R, Warren R, eds. The Shoulder and the Overhead Athlete. Philadelphia, PA: Lippincott, Williams & Wilkins; 2004: 196-208.
3.Ho CP. MR imaging of rotator interval, long biceps, and associated injuries in the overhead-throwing athlete. Magn Reson Imaging Clin N Am. 1999; 7: 23-37.
4.Clark JM, Harryman DT 2nd. Tendons, ligaments, and capsule of the rotator cuff. Gross and mi-croscopic anatomy. J Bone Joint Surg Am. 1992; 74: 713-725.
5.https://www.physio-pedia.com/Glenohumeral_Joint
6.Homsi C, Bordalo-Rodrigues M, da Silva JJ, et al. Ultrasound in adhesive capsulitis of the shoulder: is assessment of the coracohumeral ligament a valuable diagnostic tool? Skeletal Radi-ol. 2006; 35: 673-678.
7.Barber FA, Byrd JW, Wolf EM, et al. How would you treat the partially torn biceps tendon? Ar-throscopy. 2001; 17: 636- 639.
8.Bell RH, Noble JS. Biceps disorders. In: Hawkins R, Misamore GW, eds. Shoulder Injuries in the Athlete: Surgical Repair and Rehabilitation. New York, NY: Churchill Livingston; 1996: 267-282.
9.Burkhart SS, Morgan CD. The peel-back mechanism: its role in producing and extending poste-rior type II SLAP lesions and its effect on SLAP repair rehabilitation. Arthroscopy. 1998; 14: 637-640.
10.Chung CB, Dwek JR, Cho GJ, et al. Rotator cuff interval:evaluation with MR imaging and MR arthrography of the shoulder in 32 cadavers. J Comput Assist Tomogr. 2000; 24: 738-743.
11.Claessens H, Snoeck H. Tendinitis of the long head of the biceps brachii. Acta Orthop Belg. 1972; 58: 124-128.
12.Glousman RE. Instability versus impingement syndrome in the throwing athlete. Orthop Clin. North Am. 1993; 24: 89-99.
13.Harryman DT, Sidles JA, Clark JM, et al. Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990; 72: 1334-1343.
14.Fu FH, Harner CD, Klein AH. Shoulder impingement syndrome. A critical review. Clin Orthop Relat Res. 1991; 269: 162-173.
15.Petersson CJ. Spontaneous medial dislocation of the tendon of the long biceps brachii. An ana-tomic study of prevalence and pathomechanics. Clin Orthop Relat Res. 1986; 211: 224-227.
16.O'Donoghue DH. Subluxing biceps tendon in the athlete. Clin Orthop Relat Res. 1982; 164: 26-29.
17.Bennett WF, Subscapularis, medial, and lateral head coracohumeral ligament insertion anatomy. Arthroscopic appearance and incidence of "hidden" rotator interval lesions.Arthroscopy. 2001; 17: 173-180.
18.Lee J C, Guy S, Connell D, et al. MRI of the rotator interval of the shoulder. Clin Radiol. 2007; 62: 416-423.
19.Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. 1999; 8: 644- 654.
20.Habermeyer P, Magosch P, Pritsch M, et al. Anterosuperior impingement of the shoulder as a result of pulley lesions: A prospective arthroscopic study. J Shoulder Elbow Surg. 2004; 13: 5-12.