The Use of Veno-Venous Extracorporeal Membrane Oxygenation in A Patient with Recurrent Respiratory Papillomatosis Presenting with Central Airway Obstruction
Author'(s):Pui Yan Wong1 and Kin Chio Li2
1Department of Anaesthesiology, Pamela Youde Nethersole Eastern Hospital, Hong Kong.
2Department of Intensive Care, Pamela Youde Nethersole Eastern Hospital, Hong Kong.
*Correspondence:
PY Wong, 3 Lok Man Road, Chai Wan, Hong Kong SAR, China
Received: 20 August 2021; Accepted: 02 October 2021
Citation: Wong PY, Li KC. The Use of Veno-Venous Extracorporeal Membrane Oxygenation in A Patient with Recurrent Respiratory Papillomatosis Presenting with Central Airway Obstruction. Anesth Pain Res. 2021; 5(2): 1-4.
Abstract
The use of extracorporeal membrane oxygenation (ECMO) for cardio-respiratory support is increasing globally over the past decade, not only by its number of cases registered but also by the expanding list of indications. We herein report a patient with recurrent respiratory papillomatosis complicated with central airway obstruction, who presented with impeding asphyxia, and evaluate the feasibility of emergency veno- venous ECMO as a rescue therapy prior to definitive management of the primary pathology.
Keywords
Introduction
Airway obstruction is a life-threatening medical emergency in which patients can suffer from irreversible hypoxic brain damage within a short period of time. Conventional airway interventions like endotracheal intubation or front-of-neck access such as tracheostomy and cricothyroidotomy, as suggested by the Difficult Airway Society guidelines, [1] may help to relieve supra-glottic airway obstruction but not for those who suffer from distal tracheobronchial airway obstruction.
Introduced as early as the 1970s, extracorporeal membrane oxygenation (ECMO) has never come to the epicenter of the field of adults’ critical care medicine until the influenza A (H1N1) pandemic, together with the publication of a multicentered randomized controlled trial suggesting a potential survival benefit in severe respiratory failure in 2009 [2]. Since then, its indication has been expanding beyond primary respiratory or cardiac failure, with reported use in sepsis and complicated thoracic trauma [3]. Apart from maintaining oxygenation without the need of pulmonary ventilation, veno-venous (VV) ECMO facilitates airway manipulation and definitive surgical intervention in patients with complex tracheo-bronchial pathology who are deemed at risk of “can’t intubate can’t oxygenate” dilemma [4]. In this case report, we present the emergency use of VV ECMO in managing a patient with central airway obstruction and impeding asphyxia.
Case History
A 49 year-old man with known recurrent respiratory papillomatosis (RRP) requiring multiple debulking operations before, presented to the Emergency Department with acute onset of shortness of breath for three days. He had end-stage renal failure on self-continuous ambulatory peritoneal dialysis, hypertension, and history of minor stroke with full recovery.
On examination, he was mildly distressed and had audible respiratory stridor with tachypnea, SpO2 95% in room air. Flexible laryngoscopy performed by an otorhinolaryngologist revealed multiple laryngeal papillomas with tracheal involvement causing airway obstruction.
Emergency operation for papilloma debulking was booked in view of possible rapid progression of airway obstruction. On arrival to the operating theater, the patient deteriorated and developed respiratory distress requiring 10 L/min of FIO2 1.0 by Optiflow THRIVE (Transnasal Humidified Rapid-Insufflation Ventilatory Exchange) with SpO2 94%.
Because of the possible distal tracheobronchial involvement of papillomatosis and borderline respiratory condition, the patient was at considerable risk of complete airway obstruction with conventional anaesthetic management. The case was discussed by a multidisciplinary team which involved anaesthetists, intensivitis, otorhinolaryngologists, and cardiothoracic surgeons from a local tertiary hospital. Several options for airway management were considered including supraglottic jet ventilation, rigid bronchoscopy, and elective use of VV-ECMO. However, due to the lack of thoracic surgical team support in our hospital, along with the readily available ECMO team, the consensus ultimately was to initiate VV-ECMO with bi-femoral configuration, under local anesthesia. A 21 French Medtronic return cannula inserted into the right femoral vein and a 17 French drainage cannula inserted into the left femoral vein under ultrasound guidance.
General anaesthesia with a tubeless technique was commenced with intravenous remifentanil at 0.1 μg.kg-1.min-1 and target controlled infusion of propofol at the effect site concentration of 2 μg.ml-1 titrated to a bispectral index of around 40. Muscle paralysis with atracurium infusion was given. Considerable amount of recirculation was noted during the operation with desaturation. The ECMO configuration was modified with an additional 17 French drainage cannula inserted in the right internal jugular vein. The patient remained haemodynamically stable throughout the procedure even with the commencement of VV-ECMO.
At laryngo-bronchoscopy, multiple papillomatoses were found involving both the larynx and trachea with circumferential involvement, between the middle and lower part of the trachea, extending to the carina and left main bronchus, resulting in near total airway obstruction. Papilloma was removed with forceps and laryngeal microdebriders uneventfully. The patient was then intubated and transferred to the Intensive Care Unit in view of possible airway soiling.
Postoperative airway endoscopy showed no major airway obstruction and no active bleeding. ECMO was decannulated on day two post-operatively and the patient was extubated on day three. The patient was discharged from ICU to the general ward on day four. He then developed mild fluid overload and pneumonia and was successfully managed with continuous ambulatory peritoneal dialysis regimen adjustment and antibiotics. He was discharged from the hospital on day fourteen.
Outcome and follow up
One month later, the patient came back for papilloma debulking and general anesthesia with a tubeless, spontaneous ventilation method was adopted. The papilloma was found in the majority over the middle one- third of the trachea with 25% luminal obstruction, with no involvement of the carina or main bronchus.
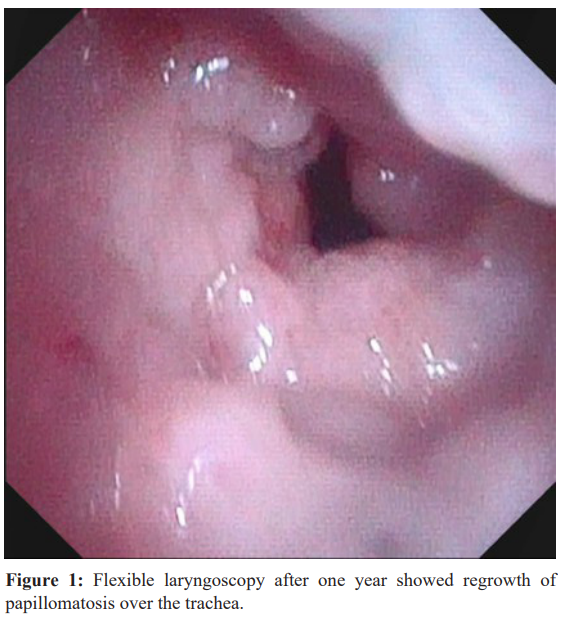
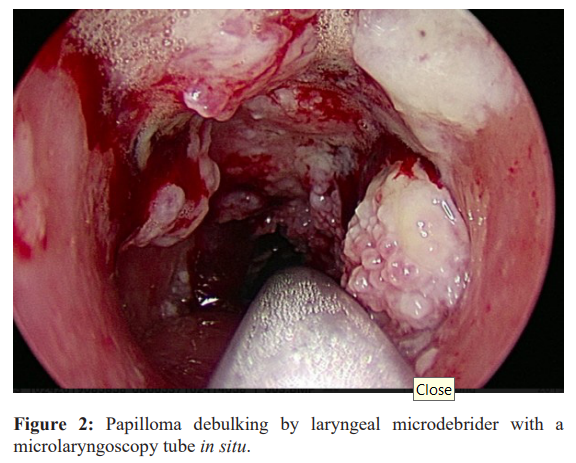
The patient required regular elective debulking operations afterwards. He came back for operation ten times over two years for his rapid regrowth of papilloma. (Figure 1) Microlaryngoscopy tube size 4 was used to facilitate debulking and the surgery was uneventful. (Figure 2) The patient was extubated and discharged to the general ward.
He suffered from aspiration pneumonia due to a previous stroke two years later and died in United Christian Hospital, Hong Kong.
Discussion
Recurrent respiratory papillomatosis (RRP) is a benign disease of the upper aerodigestive tract caused by human papillomavirus (HPV), with the commonest subtypes of HPV 6 and 11. The course of the disease varies from spontaneously resolving mild disease to aggressive disease with pulmonary spread that necessitates frequent surgical debulking and malignant transformation. There is no curative treatment, and traditional surgical treatment includes cold steel method, laser ablation (e.g. carbon dioxide, Potassium- Titanyl Phosphate (KTP), pulsed dye laser etc). However, possible complications such as airway burns with scarring, virus spreading, and airway soiling by vapour plume generation have prompted a rapid conversion to the use of laryngeal microdebriders. Adjuvant medical therapy includes intralesional cidoflovir or bevacizumab [5].
A clear and effective communication between anaesthesiologists and otolaryngologists is important in formulating a plan for airway management in shared airway surgeries. For the common approach for laryngoscope-assisted micro-debridement, intravenous general anaesthesia (IVGA) with spontaneous ventilation provides good exposure of the surgical field. However, the technique is difficult, particularly for titration of deep anaesthesia to avoid coughing, laryngospasm, and aspiration, while balancing the risk of hypoventilation. Alternatively, general anaesthesia with a tracheal tube has proven to be safe and applicable with no significant difference in terms of operation time, postoperative voice quality, or anaesthetic recovery time compared to IVGA [6]. However, the tube may interfere with surgical exposure and hinder the operation, especially those in the posterior third of the vocal cord and subglottic regions. A downsized cuffed tracheal tube can be used to maximise visualization.
In our reviewed patient, he had subglottic obstruction down to the distal airway. The greatest challenge for anaesthesia is to secure a patent airway and maintain oxygenation, and to ensure a good surgical field visibility for the procedure. It was difficult to maintain ventilatory support since the obstruction was distal to the tip of the tracheal tube. Preexisting compromised airway also predisposes to airway loss during the anesthetic induction [7]. While the use of IVGA with propofol and remifentanil, under spontaneous ventilation, has been reported in managing patients successfully with RRP resection [8], it was deemed not suitable in this particular scenario in view of such imminent total central airway obstruction with risk of airway soiling during procedure. Rigid bronchoscopy under IVGA, with intermittent positive pressure ventilation via the side port of a rigid bronchoscope, has also been performed in patients undergoing shared airway surgery with distal tracheobronchial obstruction. However, due to the unavailability of thoracic surgical team support and the critical condition of our patient, temporary respiratory support with VV- ECMO was decidedly the most favourable choice of rescuing therapy.
The use of VV-ECMO has emerged beyond its traditional indications and has established its value in shared airway procedures [9]. While oxygenation and carbon dioxide removal are ascertained with extracorporeal means, surgeons can perform high-risk surgeries with less time and space constraints, patients can benefit from lower risks of hypoventilation and hypoxia [10]. In centers that have an established capability for rapid ECMO, acute severe tracheal obstruction may be a potential indication for lifesaving procedures [11]. Extracorporeal life support should be considered as part of the algorithm for airway management and gas exchange maintenance during surgery for subtotal distal airway obstruction.
Conclusion
ECMO has evolved as a procedural support for anaesthesia and surgery with tracheobronchial interventions, not only in the intensive care setting as a rescue therapy for refractory cardio- respiratory failure. This case illustrates how with multidisciplinary input, for a patient at risk of complete central airway obstruction upon induction of anaesthesia could be safely managed with VV-ECMO.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and the accompanying images. A copy of the written consent is available for review by the Editor- in-Chief of this journal.
Data Availability
The data for this case report includes the clinical details from the anesthetic encounter as discussed in the manuscript as well as the information obtained by the cited references. There are no restrictions to data access.
Acknowledgement
We would like to thank Dr. Fergus KC Wong and Dr. Peter KC Kwan, from Department of Ear, Nose and Throat from Pamela Youde Nethersolae Eastern Hospital for their valuable opinions, and Dr. Alfred Chan Chor San from Department of Anaesthesiology from Pamela Youde Nethersole Eastern Hospital and Dr, Yam Yin Lam Jeffrey from Department of Anaesthesiology from Queen Mary Hospital for editorial assistance.
References
1.Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015; 115:827-848.
2.Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009; 374: 1351-1363.
3.Tonna JE, Abrams D, Brodie D, et al. Management of Adult Patients Supported with Venovenous Extracorporeal Membrane Oxygenation (VV ECMO): Guideline from the Extracorporeal Life Support Organization (ELSO). ASAIO J. 2021; 67: 601-610.
4.Malpas G, Hung O, Gilchrist A, et al. The use of extracorporeal membrane oxygenation in the anticipated difficult airway: a case report and systematic review. Can J Anesth. 2018; 65: 685-697.
5.Carifi M, Napolitano D, Morandi M, et al. Recurrent respiratory papillomatosis: current and future perspectives. Ther Clin Risk Manag. 2015; 11: 731-738.
6.Lei W, Wen W, Su Z, et al. Comparison of intravenous general anaesthesia vs endotracheal intubation in the surgical management of juvenile onset recurrent respiratory papillomatosis. Acta Otolaryngol. 2010; 130: 281-285.
7.Nouraei SAR, Giussani DA, Howard DJ, et al. Physiological comparison of spontaneous and positive-pressure ventilation in laryngotracheal stenosis. Br J Anaesth. 2008;101:419-423.
8.Schraff S, Derkay CS, Burke B, et al. American Society of Pediatric Otolaryngology Members’ Experience with Recurrent Respiratory Papillomatosis and the Use of Adjuvant Therapy. Arch Otolaryngol Neck Surg. 2004; 130: 1039-1042.
9.Hong Y, Jo K-W, Lyu J, et al. Use of venovenous extracorporeal membrane oxygenation in central airway obstruction to facilitate interventions leading to definitive airway security. J Crit Care. 2013; 28: 669-674.
10.Park J-H, Shin JH, Kim KY, et al. Respiratory support with venovenous extracorporeal membrane oxygenation during stent placement for the palliation of critical airway obstruction: case series analysis. J Thorac Dis. 2017; 9: 2599-2607.
11.Willms DC, Mendez R, Norman V, et al. Emergency Bedside Extracorporeal Membrane Oxygenation for Rescue of Acute Tracheal Obstruction. Respir Care. 2012; 57: 646-649.