Total Arterial Myocardial Revascularization - A One-Year Initial Experience and Literature Review
Author(s): Danko Grujic1, Aleksandar Djordjevic1,2, Radmila Karan1,3, Jelena CumiÄ?1,3, Dejan Lazovic1,2, Vladimir Milicevic1, Jacob Mulwa1 and Dusko Terzic1,2
1Clinic for Cardiac Surgery, University Clinical Center of Serbia, 11000 Belgrade, Serbia.
2Medical Faculty University of Belgrade, 11000 Belgrade, Serbia.
3Department of Anesthesiology and Intensive Care, Clinic for Cardiac Surgery, University Clinical Center of Serbia, KosteTodorovica 8, 11000 Belgrade, Serbia.
4Clinic for Cardiology, University Clinical Center of Serbia, 11000 Belgrade, Serbia.
*Correspondence:
Danko Grujic, Clinic for Cardiac Surgery, University Clinical Center of Serbia, 11000 Belgrade, Serbia.
Received: 12 May 2023; Accepted: 14 Jun 2023; Published: 19 Jun 2023
Citation: Grujic D, Djordjevic A, Karan R, et al. Total Arterial Myocardial Revascularization - A One-Year Initial Experience and Literature Review. Cardiol Vasc Res. 2023; 7(3): 1-6.
Abstract
We presented the results of the clinical outcomes of an isolated cohort of patients in whom coronary disease was treated with total arterial revascularization of the myocardium in the period of one year. We put a special focus on the preparation and use of the gastroepiploic artery as an in situ graft for revascularization of the right and posterior descending coronary arteries considering its less frequent application in cardiac surgery practice. We have shown selected reports of individual publications that we consider to unify the aforementioned strategic approach to treatment of coronary disease. According to the general trend in cardiac surgery to use minimally invasive approaches, part of the publication is dedicated to surgical revascularization through a left mini thoracotomy, where again arterial grafts are absolutely dominant.
Keywords
Introduction
Surgical myocardial revascularization has proven to be the most effective treatment of ischemic heart disease, for more than five decades, especially in conditions with complex anatomical variations and in patients with comorbidities, who have significantly influence on the choice of surgical procedure. This procedure, which was initially based on the use of exclusively venous grafts (Saphenous Vein Grafts - SVGs), significantly improved the clinical outcome with the use of an internal thoracic artery (ITA or internal mammary artery - IMA) for left anterior descending artery (LAD) revascularization. The use of the left internal thoracic artery (left internal mammary artery - LIMA) as an arterial graft for LAD shortly became the gold standard in cardiothoracic surgery. Long term results in monitoring of grafts patency, have shown that vein grafts have shorter life compared to arterial grafts. This result led surgeons to think about other options of grafts choice.
Results
In our institutions, the Cardiac Surgery Department of the Hospital in Uzice and the Cardiac Surgery Clinic of the University Clinical Center of Serbia, 153 arterial revascularization operations were performed in one year (2020 and 2021), which are presented in this paper as an isolated cohort.
Myocardial surgical revascularization was performed more often in men, who made up 71.9% (110 patients), compared to women who made up 28.1% (43 patients) of all patients. The average age of the patients operated on is 65 years, with the youngest patient being 44 and the oldest 82. One of the most important factors for the choice of procedure technique and the selection of grafts, as well as the assessment of perioperative and early postoperative risk (in terms of occurrence of wound infections) is diabetes. Preoperatively, 42 patients (26.25%) were treated for diabetes mellitus (type II), 23 of them (54.8% of all patients with diabetes) were on insulin therapy, the rest were either on combined therapy, insulin therapy and oral antidiabetics, or only on oral antidiabetics. The average value of the preoperatively estimated left ventricular ejection fraction was about 50%. In 98 patients, the operation was performed under conditions of extracorporeal blood flow (64.05%), while in 55 patients (35.9%), off-pump CABG was performed. Regarding the type of operation in terms of grafts used, the frequency of single LIMA-LAD CABG was 34 patients (22.7%). Total arterial revascularization was performed in 119 patients (78.3%). Of the total number of patients with LIMA-LAD anastomosis, in 14 the operation was performed under ECC conditions, and in 20 off- pump. In patients with total arterial revascularization, 74 were performed using extracorporeal circulation, and 45 off-pump.
During the course of treatment, neither superficial or deep infection of the sternal region was noted, nor the need for refixation of the sternum. In 23 (15%) patients, serous or sero-hemorrhagic secretion was recorded, most often from the distal half of the wound. The total number of patients with a fatal outcome is 2 (in time period of one month), which is 1.3% mortality rate of the total number of patients. One year survival were 96%.
Discussion
According to the results of our hospital and this study, total arterial revascularization proved to be an effective procedure, with favorable effects on patient survival and a shorter hospital stay. These procedures required extended time in the operating room (especially for graft preparation) compared to combined LIMA- VSM revascularization. We especially emphasize the possibility of “in situ” revascularization of posteriordescedens (Pd) branches with the gastroepiploic (GEA) as an additional advantage of this strategy. The preoperative preparation has a significant role in clinical outcomes. In standard procedures, besides Allen’s test, which is regularly done due the hospitalization, the arm CDS is included because of the valuation of ulnar and radial arterial (RA) patency. Also, in patients with important RCA stenosis revealed during the coronarography, the selective arteriography is performed, especially observing truncus coeliacus. Additional diagnostic procedures can be indicated in particularly cases. Our usual procedure was using skeletonized internal thoracic arteries, LIMA and RIMA, also RA and GEA where the sceletonization is performed up to the level before branches of both arteries. It is technically demanding procedure, which helps saving the vascularization of the thorax wall, with minimal trauma of surrounding tissue and pleura. This approach reduces the risk of superficial and deep wound infections, as well as sternum re- fixation.
Also, our “surgical goal” was strategy nonaortic off pump – as a special off pump technique with completely avoid of aortic manipulation. This procedure prevents rupture and possible athero embolization from the aorta, and consequently reduces frequency of stroke. This approach requires in situ grafts, one or both IMAs (in some cases it can be GEA), which can help to avoid aortic manipulation and proximal aortocoronary anastomosis. For total revascularization, often are needed composite T or Y anastomosis grafts, rarely as tandem or I anastomosis, if IMA requires extension with a secondary arterial graft (in most cases RA or RIMA).
As the use of IMA has become standard, other arterial grafts have become alternative solution for myocardial revascularization beyond LAD irrigation. In the 1973, Carpentier [1] with his colleagues begins to use the radial artery mainly as a free graft, because of the blood vessel lumen and thickness of the wall. After that, the choices were the right gastroepiploic artery [2] and lienal artery for revascularization of the lower myocardial parts. Total arterial revascularization still remains as an underutilized procedure in surgical myocardial revascularization.
So far, plenty studies have been done to show the impact of total myocardial revascularization on long term survival, as one of the most important parameters in monitoring of the quality of specific procedure used in treatment of ischaemic heart disease. Yanagwa and associates2 did a big meta-analysis in 2017, in which they compared total arterial myocardial revascularization with conventional coronary artery bypass grafting - CABG. Results from this meta-analysis have shown that there is statistically significant mortality reduction, for any cause, in the group of patients with total arterial myocardial revascularization (TAR) compared with non-TAR revascularization. The negative side of TAR, in cases when are used both internal thoracic arteries, is higher incidence of sternum wound infection, but also the sternum dehiscence. Although, the incidence of these complications in reported literature is less than 1% [3]. Arterial grafts, used to bridge significant coronary vessels stenoses, have histological and histochemicals characteristics that significantly differentiate them from venous grafts. Their biological performances are not unique for all available arterial grafts. They are different according to their anatomical and embryological characteristics. Those differences have impact on perioperative course and long-term graft patency.
IMA – a. mammariainterna – internal thoracic artery Location, diameter, specific histological structure and great endothelial function of IMA, make this artery the best graft choice for CABG. Both internal thoracic arteries can be used either as graft in situ or as a free graft (there can be made anastomoses with the aorta or other grafts - arterial or venous). Internal thoracic artery can be used for single blood vessels revascularization or for multiple coronary branches with one or more side-to-side anastomoses (as a sequential graft) [4]. Also, it can be pedicular graft (with accompanying veins, part of the intercostal muscles and part of the fascia), or skeletonized graft (without additional tissue). Skeletonized grafts allow utilization of the artery in her full length, with the advantage of greater initial flow [5]. This technique is less damaging for the chest walls and reduces the chance of accidental pleura opening [6]. This method is more effective because of the preservation of sternum vascularization by keeping anastomoses between the internal branches and anterior intercostal arteries, that join the posterior intercostal arteries from the thoracic aorta [7]. Furthermore, it is technically demanding procedure, especially because of the higher risk of arterial damage during the preparation from vasa vasorum. Left IMA in situ is usually used for LAD and/or diagonal branches revascularization, as single or sequential graft. This artery is rarely used as a free graft. Right IMA in situ is commonly used for revascularization of the left coronary artery branches, also for reaching the LAD across the anterior heart side or to circumflex branches behind the large blood vessels. In the first case, IMA crosses the midline over the aorta, which is a negative side in the case of re-intervention. If it is positioned over the transverse sinus, she is well protected and can reach to the distant circumflex branches, but it is more difficult to check haemostasis and can present the weak spot for the possible aortic dissection [8] (Figure 1).
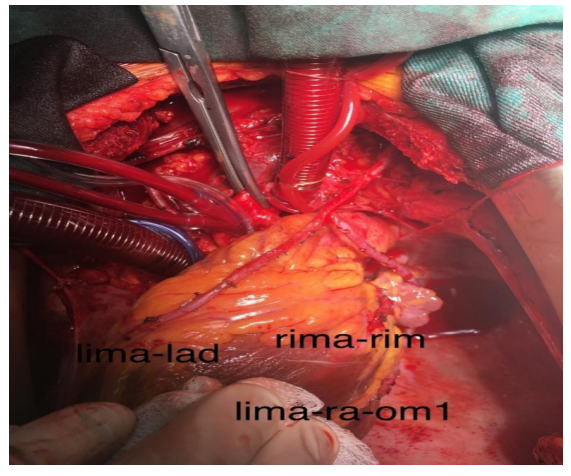
Figure 1: In situ LIMA graft for the LAD, composed T graft in situ LIMA – RA for the OM1 branch, in situ RIMA for intermediate branch.
For this reason, the common practice of positioning RIMA in situ is on the medial or distal right coronary artery (RCA), or in the case if the length of artery is enough, on posterior intraventricular artery (posterior descending artery - PDA). RIMA can be used for more distal coronary revascularization. In mostly cases, total revascularization can be achieved by using both of internal thoracic arteries, by making invert Y or T grafts or sequential grafts.
The function of IMA grafts depends on the anastomoses, the degree of stenosis and the quality of the distal part of target artery. The patency of IMA in situ on LAD is 95% after the one year, while long term follows up after 20 years shows the patency about 90% [9], but this percent is a little bit less when is the anastomosis on the another target artery. Tatoulis and coworkers done a study that included 2000 IMA with follow up for grafts patency in period of 15 years after surgery [10]. The results were decreasing graft patency during the time to 97% in case of LAD anastomosis, to 91% - 84% in case of circumflex artery or RCA.
Previous studies have shown that when a skeletonized graft is taken as whole, the long term patency of the in situ graft is equal to the patency of the LIMA. According to these studies, the patency of in situ LIMA and RIMA grafts is 97% and 95% in a period over 15 years. When there is anastomosis with the artery, which is not LAD, for example RCA, the long-term patency is a little bit less, but again, equivalently reduced as with LIMA. In the case of RIMA, used as a free graft for the left heart revascularization, in about 70% cases, the patency is less in a period of 5 years. Still, it is not statistically significant difference compared to the LIMA in situ (89% vs. 96%) [11]. In sequential grafts, where are used side-to-side anastomoses (preforming these anastomoses is more technically demanding), the graft patency has proven as remarkable, and the patency is directly correlated with the surgical technique. Control angiographs, taken in first postoperative months, showed good patency of these grafts - over 95% [12].
Radial artery - a. radialis (RA)
In recent years, the use of RA is more popular as alternative choice, because of its multiple benefits. The preparation of arterial graft is less demanding compared to the preparation of IMA, and at the same time, with lower risk of surrounding tissue complications. This graft is long enough to reach distal coronary branches and allows making multiple sequential anastomoses. Thanks to the diameter and wall thickness it is easier her use for aortic anastomosis compared to the RIMA. Because of the simpler technique, many surgeons consider RA as a second graft choice, immediately after IMA [13,14]. The RA is usually used from the left forearm, which is in most cases of the population non dominant hand. Also, it can be used from the right forearm, or from both hands, if it is necessary. The RA is used as a free graft, for proximal aortic anastomosis or other grafts. The RA is usually used for the second most important coronary artery revascularization, in patients who have contraindications for using both of IMAs. In most cases, it is used for circumflex branches or for the RCA. Rarely, can be used for diagonal branches, or in cases where neither of IMAs can be used for LAD revascularization. When the RA is long enough, it can be divided into two segments, as two free grafts [15], or can be used as a sequential graft for multiple distal anastomoses [16]. The best location for proximal anastomosis with the RA is still a question among surgeons. Many of them make direct proximal anastomosis on the ascending part of the aorta [17], while another group of surgeons uses this graft as invert Y or T proximal anastomosis on the IMA graft [18]. The second choice, allows reaching to the most distal coronary vessels, and reduces the need for the proximal aortic anastomosis (with higher risk of complications). The RA is the second choice graft, but because of the diameter and the wall thickness, it is a reason for a plenty opposite views. Many studies have shown that the short term patency is between 90 - 95%, over postoperative year or two [19,20]. In the RAPS (Radial Artery Patency Study) are observed cases where RA was used as alternative choice to venous grafts, and mainly used for circumflex or RCA anastomoses. The incidence of occluded grafts, after one year, was significantly higher in the group with venous grafts (13.6% vs. 8.9%) [21].
Gastroepiploic artery - GEA - a. gastroepiploicadexter
The GEA is usually used as graft in situ, for the revascularization of the inferior parts of the heart, most commonly for revascularization of distal RCA, PDA, rarely for marginal circumflex branches or distal LAD. (Figure 2). After in situ LIMA and RA, this graft can also be used for total arterial revascularization. In rare cases, this artery has been used in few patients for revascularization of the distal RCA or her distal branches. Usually the GEA is combined with LIMA, which is used as a graft for anterior heart wall revascularization. In these circumstances, the revascularization of the RCA is performed through the small epigastrium incision, which helps to avoid the risk of new sternotomy and venous grafting [22]. The patency of GEA, shortly after myocardial revascularization is equal to IMA. The long-term GEA patency is a little bit lower - about 80% in a period of 5 years and about 60% after 10 years. Hirose and associates [23] analyzed angiography presentations in over 1000 patients, in whom GEA was used as in situ graft for RCA revascularization. The study shown that the patency of GEA and LIMA was 98% and 99% after one year, and 84% and 97% after three years. It should be in mind that the study was performed in patients with recurrent angina and that in this patients GEA was used for RCA and her branches revascularization, with less patency - short or long term (Figure 3). It is important to know that the degree of stenosis has a big impact on the long-term graft function, as best demonstrated by GEA (revascularization of mid-degree stenosis). Using GEA as a native graft in cardiothoracic surgery is still an issue, basically because of the technical training and experience of surgeons, which is reflected in the need for bigger incision for abdominal cavity approach, the preparation of the graft, opening the diaphragm and eventually making of anastomoses. Besides that, there is also a question about possible complications, like possibly compromised gastric vascularization because of the partial deprivation of gastric arterial flow. So far, studies or surgeon experiences did not show increasing perioperative morbidity or mortality [24]. Long term clinical results of using GEA (using one or more arterial grafts), have proven as excellent, without new ischemic complications in more than 80% of cases, over 10 years [25]. GEA is rarely used as a free graft, and because of the big diameter can be anastomozed with the ascending part of the aorta or as composite arterial graft, proximal on the IMA or RA.

Figure2: In situ RGEA, prepared, performed grafting through a previously prepared space on the diaphragm, planned anastomosis for the Pd branch.
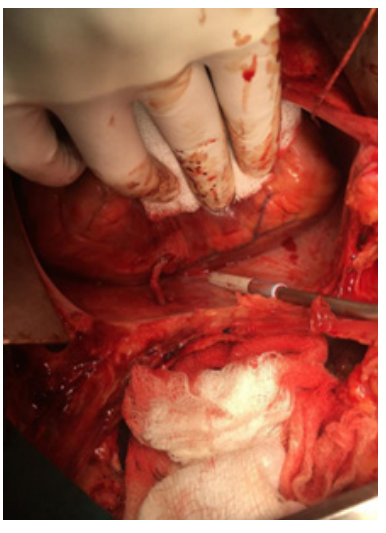
Figure 3: In situ right GEA anastomosis for Pd branch.
The off pump CABG and Minimally Invasive Surgical Revascularization of the Heart
The CABG off pump in surgical myocardial revascularization has been used for over 30 years. Benefits of the off pump are avoiding potential trauma, which can be result of the cardiopulmonary bypass and minimal aortic manipulation. Many of studies shown that use of this pump reduced the early mortality and perioperative neurological disorders, renal failure, blood transfusions and number of hospitals days after the intervention. The negative side of this pump are mainly related with incomplete and/or lower quality myocardial revascularization, which potentially can increase number of recurrent re-interventions and late mortality. Despite 3 decades, 115 randomized studies, more than 60 meta analyzes comparing on and off pumps, the role and indications of the CABG off pump, remains a controversy. The CABG off pump according to many studies has a significant advantage compared to on pump, because of the activation of several pathophysiological pathways at the molecular level. These pathways are reflected through the systemic inflammatory response, platelets activation, activation of coagulation system and increasing oxidative stress and endothelial dysfunction. These changes can happen either after the on and off pump, while some pathways are more potent in CPB [26]. The aim of the CABG off pump is completely excluding the CPB from the procedure, because of the reducing bigger inflammatory response, which can have impact on decreased rate of systemic organ failures and damages (renal, cerebral and neurological disorders). In most cases, CABG procedure was based on the use of in situ LIMA grafts for LAD and at least one proximal aortocoronary venous graft placed on the ascending part of the aorta, by using a partial occlusion clamp. The trend of modern cardiac surgical practice implies the more frequent application of minimally invasive procedures. Mini thoracotomy myocardial revascularization (MIDCAB) is an effective cardiac surgical method with good clinical results in patients where the coronary anatomy and atherosclerotic pathological process allow the cardiac surgeon adequate access to the areas of the myocardium where it is optimal to create an astomoses on the coronary arteries. Faster postoperative recovery of the patient and a superior cosmetic effect using this method of myocardial revascularization have been proven. MIDCAB is part of apersonalized CABG performance strategy (Figure 4).
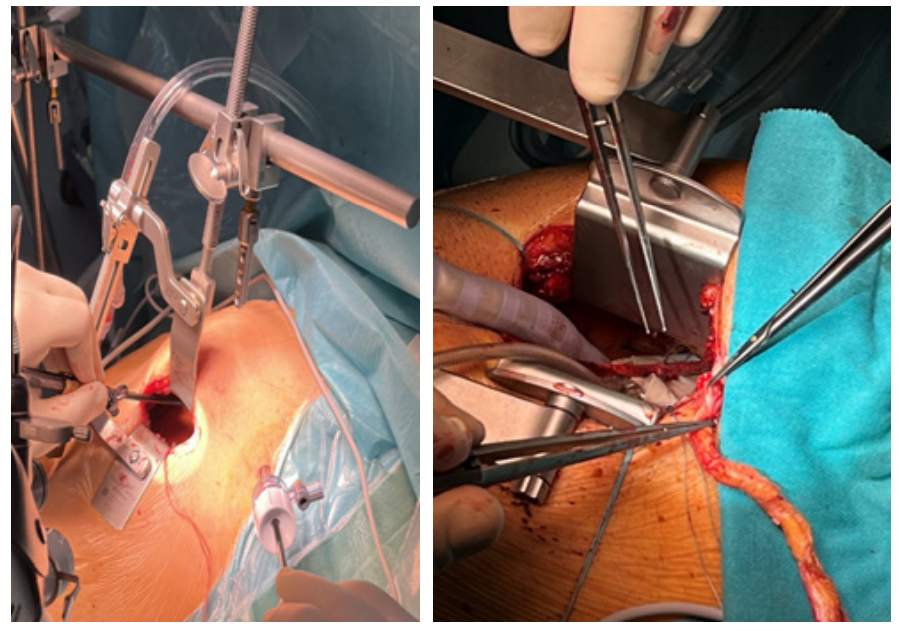
Figure4: MIDCAB procedure preparation of LIMA (left) and anastomosis to LAD (right).
Conclusion
Total arterial revascularization is a safe procedure with excellent results. Potential challenges related to aortic pathology, ischemic changes in the lower extremities, or limitations in the use of extra corporalblod flow can be successfully overcome with this strategy. The benefits of this procedure, especially in young patients, are invaluable. When it comes to TAR, the severe complications as the frequency of superficial and deep wound infections (less than 1% in the literature), can be prevented by appropriate preoperative preparation, adequate surgical technique (skeletonization of the IMA), and valid postoperative wound care. Total arterial revascularization has become a wide use standard procedure in our hospital with a tendency to be predominantly nonaortic CABG off pump. Total arterial revascularization is demanding procedure for the surgeon, because of the longer time spent in the OR, the extreme patience and physical condition of the surgeon, as well as good technique for graft preparation and making anastomosis on the beating heart. Regardless, this intervention represents more benefits in short and long term clinical outcomes in the treatment of coronary disease.
References
- Carpentier A, Guermonprez JL, Deloche A, et al. The aorta- to-coronary radial artery bypass grafs.AnnThorac Surg. 1973; 16: 111-121.
- Pym J, Brown PM, Charette EJ. Gastroepiploic coronaryanastomosis. J ThoracCardiovasc Surg. 1987; 94: 256-259.
- Yanagawa B, Verma S, Mazine A, et al. Impact of total arterial revascularization on long-term survival: A systematic review and meta-analysis of 130,305 patients. International Journal of Cardiology. 2017; 233: 29-36.
- Deja MA, Wos S, Golba K, et al. Intraoperative and laboratory evaluation of skeletonized versus pedicled internal thoracic artery. AnnThorac Surg. 1999; 68: 2164-2168.
- Takami Y, Ina H. Effects of skeletonizacion on intraoperative flow and anastomosis diameter of internal thoracic arteries in coronary artery bypass grafting. Ann Thorac Surg. 2002; 73: 1441-1445.
- Matsumoto M, Konishi Y, Miwa S, et al. Effect of different methods of internal thoracic artery harvest on pulmonary function. Ann Thorac Surg. 1997; 63: 653-655.
- Lorberboym M, Medalion B, Bder O, et al. 99Mtc-MDP bone SPECT for the evaluation of sternal ischaemia following internal mammary artery dissection. Nucl Med Commun. 2002; 23: 47-52.
- Accola K, Jones E, Craver J, et al. Bilateral mammary artery grafting: avoidance of complicationswith analysis. Ann Thorac Surg. 1993; 56: 872-879.
- Sah PJ, Durairaj M, Gordon I, et al. Factors affecting patency of internal thoracic artery graft: clinical and angiographic study in 1.434symptomatic patients operated between 1982- 2002. EurJCardiothorac Surg. 2004; 26: 118-124.
- Tatoulis J, Buxton BF, Fuller J. Patencies of 2,127 arterialto coronary conduits over 15 years. Ann Thorac Surg. 2004; 77: 93-101.
- Tatoulis J, Buxton BF, Fuller JA. Results of 1,454 free internal thoracic artery-to-coronary artery grafts. Ann ThoracSurg. 1997; 64: 1263-1268.
- Dion R, Glineur D, Derouck D, et al. Long-term clinical and angiopraphic follow-up of sequential internal thoracic artery grafting. EurJCardiothorac Surg. 2000; 17: 407-414.
- Tatoulis J, Royse A, Buxton BF, et al. The radial artery in coronary surgery: a5-year experience-clinical and angiographic results. AnnThorac Surg. 2002; 73: 143-148.
- Caputo M, Reeves B, Marchetto G, et al. Radial versus right internal thoracic arteryas a second arterial conduit for coronary surgery: earlyand midterm outcomes. J Thorac Cardiovasc Surg. 2003; 126: 39-47.
- Barner HB. Defining the role of the radial artery. Semin Thorac Cardiovasc Surg. 1996; 8: 3-9.
- Weinschelbaum EE, Gabe ED, Macchia A, et al. Total myocardial revascularization with arterialconduits: radial artery combined with internal thoracic arte-ries. J Thorac Cardiovasc Surg. 1997; 114: 911-916.
- Tatoulis J, Buxton BF, Fuller JA. Bilateral radial artery grafts in coronary reconstruction. Technique and early results in 261 patients. Ann Thorac Surg. 1998; 66: 714-720.
- Calafiore AM, di Giammarco G, Teodori G, et al. Radial artery and inferior epigastricartery in composite grafts: improved midterm angiographic results. Ann Thorac Surg. 1995; 60: 517-523.
- Tector AJ, Amundsen S, Schmahl TM, et al. Total revascularization with T grafts. Ann Thorac Surg. 1994; 57: 33-39.
- Maniar HS, Barner HB, Bailey MS, et al. Radial artery patency: are aortocoronaryconduits superior to composite grafting?. Ann Thorac Surg.2003; 76: 1498-1504.
- Iaco AL, Teodori G, di Giammarco G, et al. Radial artery for myocardial revascularization: Long-term clinical and angiographic results. AnnThorac Surg. 2001; 72: 464-469.
- Grandjean JG, Mariani MA, Ebels T. Coronary re-operation via small laparotomy using the right gastro-epiploic artery without cardiopulmonary bypass. Ann Thorac Surg. 1996; 61: 1853-1855.
- Hirose H, Amano A, Takanashi S, et al. Coro-nary artery bypass grafting using the gastroepiploic artery in 1,000 patients. Ann Thorac Surg. 2002; 73: 1366-1367.
- Suma H, Wanibuchi Y, Furuta S, et al. Does thegastro-epiploic artery graft increase surgical risk? J ThoracCardiovasc Surg. 1991; 101: 121-125.
- Endo M, Nishida H, Tomizawa Y, et al. Beneditofbilateral over single internal mammary artery grafts formultiple coronary artery bypass grafting. Circulation. 2001; 104: 2164-2170.
- Antoniades C, Demosthenous M, Reilly S, et al. Myocardial redox state predicts inâ?hospital clinical outcome after cardiac surgery effects of shortâ?term preâ?operative statin treatment. J Am CollCardiol. 2012; 59: 60-70.