Translating Results from The Womed Model of Benign Thyroid Disease to A Practical Approach to Treat Fatigue In COVID-19 Patients Based on Combined Supplementation with Magnesium, Selenium, and Coenzyme Q10: A Treatment Strategy against Fatigue
Author'(s): Moncayo Roy* and Moncayo Helga
WOMED, Private Practice, Karl-Kapferer-Strasse 5, 6020 Innsbruck, Austria.
*Correspondence:
Roy Moncayo, WOMED, Private Practice, Karl-Kapferer-Strasse 5, 6020 Innsbruck, Austria, E-mail: Life-RM@outlook.com.
Received: 17 November 2020; Accepted: 02 December 2020
Citation: Moncayo R, Moncayo H. Translating Results from The Womed Model of Benign Thyroid Disease to A Practical Approach to Treat Fatigue In COVID-19 Patients Based on Combined Supplementation with Magnesium, Selenium, and Coenzyme Q10: A Treatment Strategy against Fatigue. Cardiol Vasc Res. 2020; 4(5): 1-4.
Abstract
We describe a small series of patients who were examined at a time post-COVID-19 infection. The main common complaint at presentation was fatigue. Using a previously described and clinically validated examination method based on 3D-Power Doppler sonography of the thyroid, we could identify signs of coenzyme Q10 (CoQ10) deficiency in these cases. In our previous investigations we have been able to correlate CoQ10 deficiency with a metabolic switch to glycolysis, i.e. a biochemical process with low ATP production output. Combined supplementation with magnesium, selenomethionine and CoQ10 improved the clinical condition. Signs of CoQ10 deficiency persisted in 2 cases where stress situation through workload persisted. Stress is a condition associated with low levels of CoQ10. We propose that CoQ10 deficiency can be involved in the pathogenesis of COVID-19 infection affecting physical performance, and potentially also heart function resulting in fatigue. Experimental and clinical data from the literature on the use of CoQ10 suggest that this compound should be considered in treatment strategies for COVID-19 patients
Keywords
Introduction
Fatigue is a symptom that can persist in thyroid disease patients who are receiving an adequate treatment as evidenced through thyroid hormone levels. This clinical discrepancy, which is vital for the well-being of patients, motivated us to search for an explanation and treatment for this condition. Through a series of observational studies, we have developed a disease concept related to fatigue where key biochemical deficiencies of magnesium, selenium, and coenzyme Q10 lead to a state of acquired mitochondrial dysfunction [1,2]. In daily clinical practice, this situation can be easily recognized by examining the thyroid with advanced ultrasound techniques such as 3D-power Doppler sonography [3].
Once the condition is detected, it can be easily be corrected through supplementation resulting in restitution of thyroid morphology [4], thus reverting the primary disease condition.
In 2020 we have added 2 new features to benign thyroid disease: 1) the recognition of a glycolytic metabolic condition of the thyroid and the heart, and 2) importance of magnesium in lowering the levels of anti-thyroglobulin antibodies. Glycolysis as a source of ATP production is known to be less efficient than the process of oxidative phosphorylation. This means that ATP availability in the body is reduced thus affecting physical performance. At the same time less ATP will affect restitution processes in the body related to the endoplasmic reticulum and protein quality control since elements of the unfolded protein response depend on ATP. A description and discussion of these biochemical changes can be found in our recent publication [5].
Although our practice is not primarily involved in the primary treatment of patients with COVID-19, we have had the opportunity to study a small number of patients presenting post-COVID-19 fatigue.
Patients and Methods
Between November and December 2020, we have examined 3 female patients who had had COVID-19 disease and whose main presenting complaint was fatigue and loss of physical performance. Their present performance level corresponded to 70 to 80% less than before. This figure was extracted through clinical history in relation to achievement level of athletic performance, i.e. swimming and running distances. The diminished physical performance ability was also noticeable in conducting everyday tasks which had become cumbersome.
The main examination tool was 3D-Power Doppler sonography of the thyroid. When the sonography signs suggested the condition of biochemical deficiency of magnesium, selenium and CoQ10, a combined supplementation was prescribed. Patients were followed-up every 2 weeks. The supplementation plan included the following: 1) 4g of pure magnesium citrate powder to be dissolved in water (750ml) and taken during the day, 2) selenomethionine 200 µg capsules, and 3) CoQ10 60mg capsules; both preparations were from Pure Encapsulations. The initial dose for selenium and CoQ10 is one capsule at bedtime for 2 weeks. Beginning on the third week, the dose is reduced to 1 capsule of each preparation taken on alternate days 3 times per week.
Results
Case 1 – The Index Case
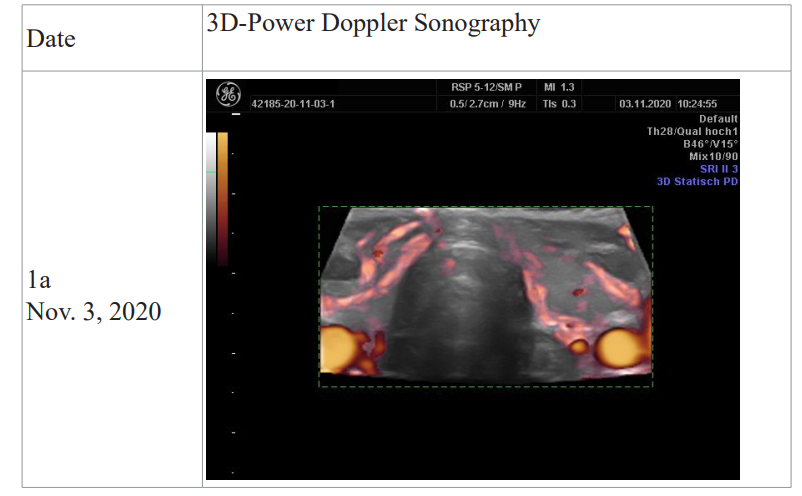
The 3D power Doppler examination revealed the same pattern of altered thyroid gland perfusion which we have previously identified as being a sign of CoQ10 deficiency. The first examination revealed a pure CoQ10 deficiency pattern; only wide vessels were evident (Figure 1a). One week later a slight flare-up was seen (Figure 1b). Four weeks later hyper-perfusion was clearly reduced (Figure 1c). At the same time fatigue had disappeared and physical performance had returned to normal.
Case 2 – A Relapse case
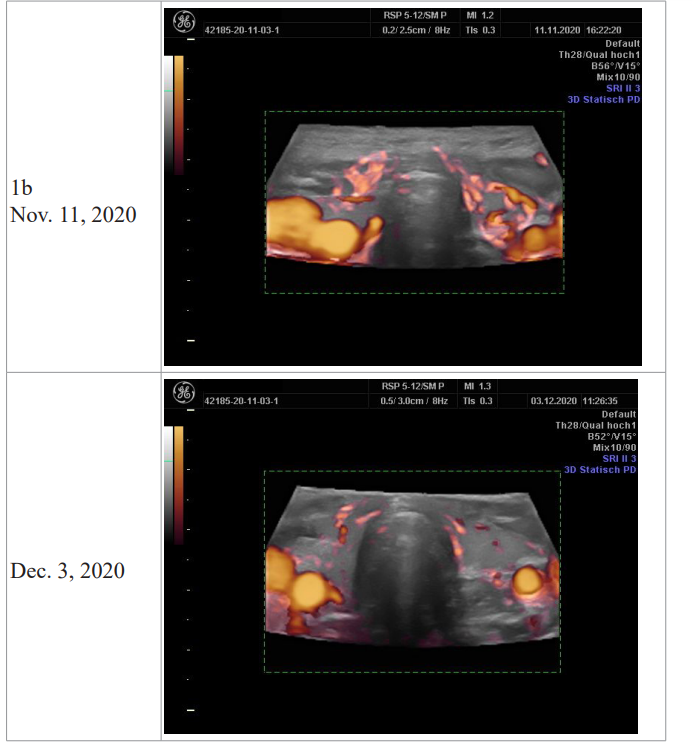
At the time of presentation hyper-perfusion was only slightly increased. Four weeks later the perfusion pattern was more intense, and the performance level was reduced by 20%. This relapse situation occurred when the COQ10 dose was taken on alternate days. An additional factor influencing this situation was an increased workload and stress. After the examination daily intake of CoQ10 was re-started.
Case 3 – A persisting case
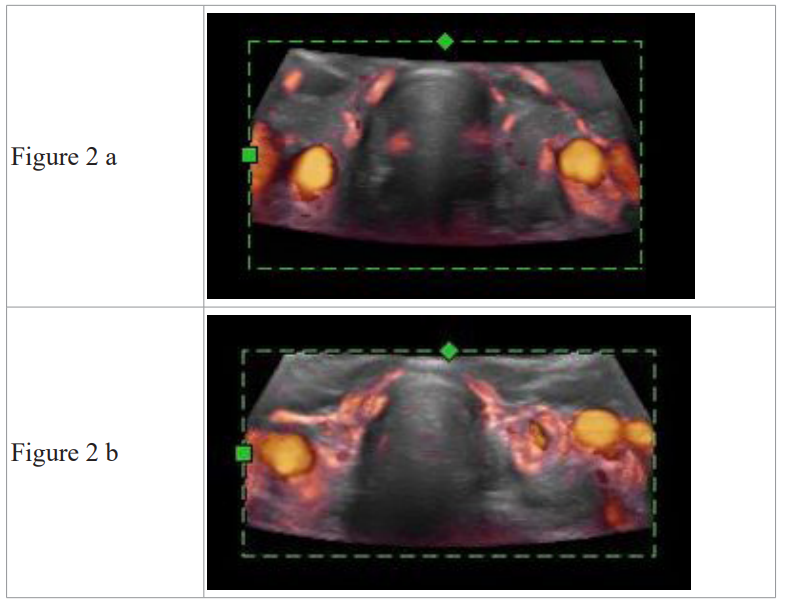
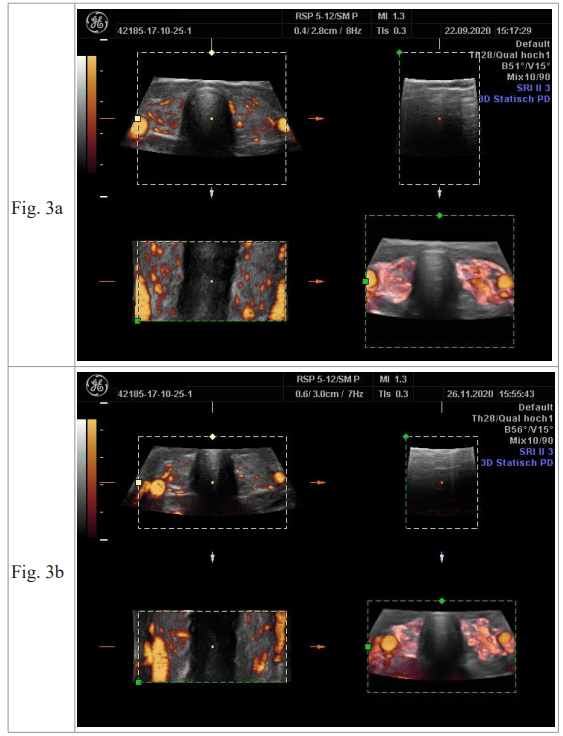
This case showed a partial improvement of magnesium deficiency; however the condition of CoQ10 deficiency was persistent 7 weeks later. The third case of the series is shown in a 3-volume view of the 3D-Power Doppler thyroid sonography. In Figure 3a the upper left panel shows the signs of magnesium deficiency which produce a fine granular perfusion pattern. The lower right panel shows the 3D image corresponding to widened vessels, i.e. CoQ10 deficiency. In Figure 3b the signs of magnesium deficiency are less evident, while CoQ10 deficiency persists. Physical performance level at this time was reduced by 30%.
Discussion
Our ultrasound examination procedure of the thyroid, based on 3D power Doppler technique, has allowed us to identify perfusion patterns in the gland that correspond to a CoQ10 deficiency state in patients who had had active COVID-19 disease and were complaining of fatigue or diminished physical capacity. Sequential follow-up of our index case during 4 weeks of combined supplementation revealed a gradual resolution of the changes in ultrasound and at the same time physical fitness returned to a normal level. Due to persisting stress situations at work, cases 2 and 3 did not show a resolution of CoQ10 deficiency, while magnesium deficiency was less pronounced.
We propose that CoQ10 is an essential element of the oxidative phosphorylation chain that is affected in COVID-19 patients as in thyroid disease patients [2,5]. A comparison with medical literature is not possible since similar evaluations have not been carried out. Under experimental conditions studying viral myocarditis in mice, Kishimoto et al. have shown a protective and beneficial effect of CoQ10 administration [6]. Rosenfeldt et al. have also proposed a protective role for CoQ10 against stress in the aging heart [7].
While the exact mechanism leading to CoQ10 deficiency cannot be elucidated now, we would like to conclude this communication citing the experimental work of Liparulo, Bergamini, et al. who have studied the pathogenic mechanisms behind CoQ10 deficiency [8]. They propose that CoQ10 deficiency results in increased cellular cholesterol content which reduces plasma membrane fluidity leading to lower oxygen diffusion while at the same time glycolysis is stimulated and ATP production reduced. In a clinical investigation Khan et al. have recently shown that CoQ10 administration to patients scheduled for vascular surgery can improve the clinical outcome while at the same time the levels of NT-proBNP - a marker for cardiac damage - can be lowered [9].
We conclude that alterations of CoQ10 metabolism and function can be expected to be found in COVID-19 patients resulting in clinical signs of fatigue and potentially affecting patients with previous known cardiac disease, a condition where COQ10 deficiency is known to exist [10]. Adding this compound to treatment strategies would improve the quality of life of the patients and improve their outcome.
References
- Moncayo R, Moncayo H. Exploring the aspect of psychosomatics in hypothyroidism: the WOMED model of body-mind interactions based on musculoskeletal changes,psychological stressors, and low levels of magnesium. Woman - Psychosomatic Gynaecology and Obstetrics. 2014; 1: 1-11.
- Moncayo R, Moncayo H. The WOMED model of benign thyroid disease: acquired magnesium deficiency due to physical and psychological stressors relates to dysfunction of oxidative phosphorylation. BBA Clin. 2015; 3: 44-64.
- Moncayo R, Moncayo H. Advanced 3D sonography of the thyroid: focus on vascularity. In: Thoirs K, editor. Sonography. http://www.intechopen.com/articles/show/title/thyroid-sonography-in-3d-with-emphasis-on-perfusion.1ed.Rijeka,Croatia:Intech.2012;273-292.
- Moncayo R, Moncayo H. Proof of concept of the WOMED model of benign thyroid disease: Restitution of thyroid morphology after correction of physical and psychological stressors and magnesium supplementation. BBA Clin. 2015; 3: 113-122.
- Moncayo R, Moncayo H, Reisenzahn J. Global view on the pathogenesis of benign thyroid disease based on historical, experimental, biochemical, and genetic data identifying the role of magnesium, selenium, coenzyme Q10 and iron in the context of the unfolded protein response and protein quality control of thyroglobulin. Journal of Translational Genetics and Genomics. 2020; 4: 1-27.
- Kishimoto C, Tomioka N, Nakayama Y, et al. Anti-oxidant effects of coenzyme Q10 on experimental viral myocarditis in mice. J Cardiovasc Pharmacol. 2003; 42: 588-592.
- Rosenfeldt FL, Pepe S, Linnane A, et al. Coenzyme Q10 protects the aging heart against stress: studies in rats, human tissues, and patients. Ann N Y Acad Sci. 2002; 959: 355-465.
- Liparulo I, Bergamini C, Bortolus M, et al. Coenzyme Q biosynthesis inhibition induces HIF-1α stabilization and metabolic switch toward glycolysis. FEBS J. 2020.
- Khan A, Johnson DK, Carlson S, et al. NT-Pro BNP Predicts Myocardial Injury Post-vascular Surgery and is Reduced with CoQ10: A Randomized Double-Blind Trial. Ann Vasc Surg. 2020; 64: 292-302.
- Folkers K, Littarru GP, Ho L, et al. Evidence for a deficiency of coenzyme Q10 in human heart disease. Int Z Vitaminforsch. 1970; 40: 380-390.