Two-Year Incidence of Permanent Pace-Maker Implantation Post Modified SAVR
Author'(s): Nadine Kawkabani MD1*, Omar Boustros MD2, Rita Farah PharmD3, Rola Darwish MD1, Moussa Abi Ghanem MD2, Jennifer Jdaidani MD2 and Bassam Abu Khalil MD2
1Department of cardiac surgery anesthesia, St Georges HospitalUniversity Medical center, Beirut, Lebanon.
2Department of Cardiothoracic Surgery, St Georges HospitalUniversity Medical center, Beirut, Lebanon
3Balamand University, Lebanon.
*Correspondence:
Nadine Kawkabani MD, Department of cardiac surgery anesthesia, St Georges Hospital-University Medical center, Beirut, Lebanon, Tel: +961 (3) 548467.
Received: 10 Apr 2022; Accepted: 15 May 2022; Published: 20 May 2022
Citation: Kawkabani N, Boustros O, Farah R, et al. Two-Year Incidence of Permanent Pace-Maker Implantation Post Modified SAVR. Cardiol Vasc Res. 2022; 6(3): 1-4.
Abstract
Background and Aim of this Study: Patients presenting with aortic stenosis are offered surgical aortic valve (SAVR) or transcatheter aortic valve replacement (TAVR) as therapeutic options. However, both techniques are associated with postoperative conduction abnormalities necessitating PPMI.
We evaluate in this paper the impact of a modified technique of SAVR- which aims to decrease the stress on the conduction system- on the incidence of PPMI for a 24 months period post-surgery.
Methods: The perioperative course of 184 patients who underwent SAVR in Saint George Hospital University Medical center between January 2016 and June 2019 was assessed.
The study compares the incidence of PPMI between two groups of patients. In group A, 92 patients underwent the classic SAVR and in-group B, and 92 patients underwent a modified SAVR.
Results: The results revealed a significant decrease of PPMI from 12 to 2.2% during a two-year period follow up. A multi variate analysis showed that the modified technique was a strong predictor for PPMI post SAVR. In addition, this rate (2.2%) was lower than the ones reported after TAVR.
Conclusion: This reproducible and reliable technique should be recommended whenever SAVR is performed. On the other hand, the low incidence observed may be adopted as a benchmark whenever TAVR is offered as a therapeutic option specially to intermediate and low risk patients. Moreover, this less traumatic technique should be retained whenever stent design modifications for TAVR are considered.
Keywords
Introduction
A significant increase in the number of patients referred for aortic valve replacement (AVR) has been noticed in the recent years [1].
Patients presenting with aortic stenosis are offered surgical aortic valve (SAVR) or trans catheter aortic valve replacement (TAVR) as therapeutic options. However, both techniques are associated with postoperative conduction abnormalities necessitating permanent pace maker implantation (PPMI).
Numerous papers reported that 2-7% of patients undergoing SAVR need PPM insertion while a larger percentage of patients need PPMI post TAVR [2-5].
Many factors have been implicated in increasing the risk of AV block and subsequent PPMI. The stress on the conduction system seems to be a major cause of this complication [1-6].
In this present paper, we evaluate the impact of a modified SAVR-, which aims to decrease the preoperative trauma of the conduction system- on the incidence of PPMI for a 24 months period post-surgery.
Methods
The perioperative course of 184 patients who underwent surgical biological aortic valve replacement in Saint George Hospital University medical Center between January 2016 and June 2019 was assessed and a follow-up was performed up to 24 months post operation. The institutional review board (IRB) at Saint George University Medical Center approved the study.
Population
Participants were divided into two groups: Group A that included 92 patients who underwent the classic technique of AVR between January 2016 and June 2017 and group B that included 92 patients who underwent a modified technique of AVR between July 2017 and June 2019.
Data Collection
A cardiothoracic surgery resident extracted basic demographics, past medical history, clinical, Para clinical and laboratory data (Arterial blood gases electrolytes, calcium… from patients’ medical records. Patients were evaluated after obtaining an informed consent, before surgery, immediately postoperatively and for a period of 24 months after surgery.
Operative Technique
One surgeon performed all surgical cases. Biological aortic valve replacement was performed for the clinical indication of AVR such as aortic stenosis, calcifications… Participants were divided into two groups: Group A that included 92 patients who underwent the classic technique of AVR between January 2016 and june 2017 and group B that included 92 patients who underwent a modified technique of AVR between july 2017 and june 2019.
Demographic and characteristics data are shown in table1.
In the classic technique of AVR, the surgeon used pledgeted 2.0 ethibond with the pledgets applied below the annulus while in the modified technique the same 2.0 pledgeted ethibond were put below the annulus except for 3-4 sutures at the commissure between the right and non-coronary sinuses. They were applied above the annulus (Figure1).
Postoperative Follow up
All patients were closely followed in the immediate postoperative period and for a 24 months period after surgery. Postoperative conduction disturbances and subsequent implantation of permanent pacemaker were studied throughout this period. Other complications such as hemodynamic instability and electrolytes imbalance were also analyzed.
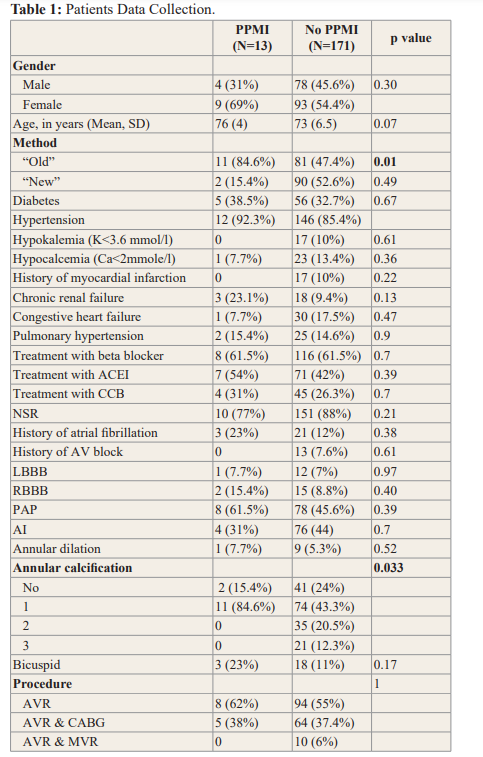
ACEI: Ace Enzyme Inhibitor, CCB: Calcium Channel Blocker, NSR: Normal Sinus Rhythm, AV: Atrioventricular, LBBB: Left Bundle Branch Block, RBBB: Right Bundle Branch Block, PAP: Pulmonary Artery Pressure, AI: Aortic Insufficiency, AVR: Aortic Valve Replacement, CABG: Coronary Artery Bypass, MVR: Mitral Valve Replacement.
Statistical Analysis
We used the SPSS software version 23.0 for data analysis. We used means with standard deviations and percentages to describe continuous and categorical variables, respectively. We used the Pearson chi-square (X2) test to compare categorical variables and we used Fisher exact test when the expected values within cells were <5. We used the Student’s t-test to compare means between two groups. A p value <0.05 was considered statistically significant. We performed a multivariable analysis using a binary logistic regression model to study the association between the surgical technique used and the need for pacemaker after adjusting for confounders.
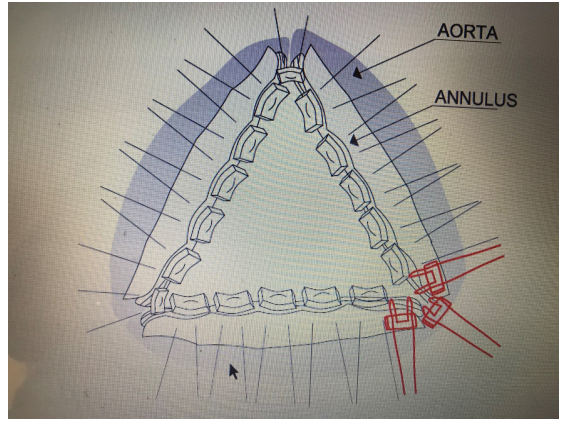
Figure 1: 3-4 sutures were applied above the annulus at the commissure between the right and non-coronary sinuses.
Results
Postoperatively, the incidence of complete atrioventricular (AV) block was significantly higher in-group A and reached 12% compared to 2.2% in-group B. To note that in group A, 9 patients required a pace maker in the immediate postoperative period while 2 patients developed a third-degree block three months after surgery necessitating hospitalization and pace maker implantation. In-group B, the two patients who needed a pace maker developed the AV block in the immediate post-operative course. No late conduction abnormalities were observed during the 24 months follow up.
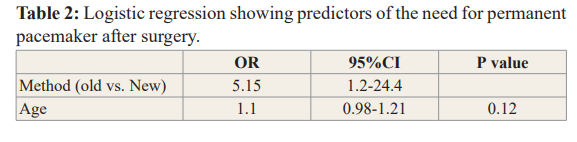
The univariate analysis showed that patients who needed the implantation of a PPM were significantly older than those who did not require a PPM post operation (76 ± 4 years vs. 73 ±6.5 years). Multivariable analysis showed that the operative technique was a strong predictor of the need for permanent pacemaker implantation after adjustment for patients’ age (OR 5.15; 95% confidence interval 1.2-24.4). The odds of needing pace maker implantation were 5 times higher among patients in group A as compared to patients in group B (Table 2).
Discussion
Patients presenting with aortic stenosis are offered SAVR or TAVR. Both techniques are associated with postoperative conduction abnormalities necessitating implantation of PPM. Many papers reported that 2-7% of patients require permanent pacing after surgical aortic valve replacement while a larger percentage (6- 34%) of patients need PPMI following TAVR [1-4].
Numerous factors have been incriminated in increasing the incidence of complete AV block such as age, preoperative rhythm abnormalities, myocardial infarction, use of beta blockers, calcium channel blockers, perioperative electrolytes imbalance, surgery for AI and long bypass [5,6]. Klapkowzki et al. reported that PPMI following isolated SAVR was required in 6.1% of cases of all analysed clinical, anatomical and surgical factors prolonged cardiopulmonary bypass and aortic cross clamp time, larger size of the implanted valve prosthesis; endocarditis and electroloyte disturbances were found to be statistically significant predictors of permanent pacemaker implantation [3]. In contrast, Nardi et al. found that the incidence of PPMI was similar for patients either with or without preoperative conducting system disease [7].
Dizone et al. reported on March 2019 that the rate of PPMI during a period of 10 days post-surgery was 6.1% following SAVR versus 9.3% following TAVR. Two-year prevalence was 11% after SAVR versus 13% post TAVR. The most important risk factor for PPMI was preoperative BBB either right or left. Atrial fibrillation and enlarged LVED dimension were among risk factors for PPM in the constant hazard phase [8].
In our study, after analyzing all the variables that have been incriminated in increasing the need for PPMI post AVR, we found that the surgical technique was a very strong predictor of PPMI while preoperative conduction abnormalities and atrial fibrillation did not seem to affect the incidence of PPMI. To note that the prevalence of PPMI-in contrast to the results described by Dizone et al. remained constant throughout the two-year follow up period in the group of patients who underwent the modified surgical AVR.
The complete AV block per se may be due to direct trauma and stress to the conduction system while performing SAVR or TAVR. In fact, trauma may occur during SAVR while performing debridement of severely calcified valves or while placing the sutures especially in the triangular area that embeds the conduction system. On the other hand, injury may be attributed, during TAVR to radial forces that are usually exerted on the conduction system. Nardi et al. discussed the impact of surgical techniques earlier. They found that an accurate technique for debridement of calcific material may help preventing further impairment of the conduction system and subsequently results in decreasing PPM insertion [7].
In our manuscript, we described a modified surgical technique of biological AVR that minimizes the stress on the conduction system and we studied the impact of this technique on the incidence of PPMI for a two-year period post-surgery.
In a previous study, we observed a significant decrease of PPMI (3.2 versus 14.5%) in the group of patients who underwent the modified technique one month after surgery [9]. In this paper, the results showed a further decrease of the incidence of PPMI (2.2%versus 12%) during a two- year follow up. The odds of needing PPMI were five times higher among patients who underwent the classic technique of AVR as compared to patients who underwent the modified technique.
TAVR has emerged as an alternative treatment for patients with severe aortic stenosis replacement and has been adopted increasingly all over the world. Since 2002, it has been offered to non-operable candidates or to patients who were at high risk for AVR. In the last years, it has been considered as a therapeutic option to intermediate and even to low-risk patients. However, TAVI has been associated with a high incidence of PPMI. The frequency of new PPM needed post procedure varied based on the valve system and was significantly lower with the balloon expandable valves than the self-expanding ones. Meta-analysis studies reported that implantation of PPM rates ranged from 5.9% to 6.5% when balloon expandable valves were used and from 24.5 to 28.8% when self-expandable valves were inserted. The higher rate of new PPM with self-expandable materials was likely due to differences in stent design and properties that influence the position of the valve frame within the LVOT and the radial force exerted on the conduction system. The PARTNERS study analyzed the data of 1973 patients who underwent TAVR. PPMI was required in 8.8% of patients who underwent TAVR with a balloon expandable valve. Preexisting RBB, the prosthesis to LV outflow tract diameter ratio and LVEnd diameter were identified as novel predictors of PPM need after TAVR. New PPM cases were associated with a larger duration of hospitalization and higher rates of repeated hospitalization at one year and mortality [3,10].
In our paper, the rate of PPMI in the group of patients who underwent the modified technique decreased significantly to 2.2%. This low incidence, which seemed to remain stable two years after surgery, is inferior to the rate of PPMI following TAVR, whether self-expandable or balloon expandable valves are used. This may be attributed mainly to the decrease of trauma on the conduction system while placing the valve.
Conclusion
The sustainable low incidence of PPMI (2.2%) following modified surgical biological AVR encourages us to recommend this reproducible and reliable technique to all patients undergoing SAVR.
On the other hand, modified SAVR minimizes the stress on the conduction system leading to significant decrease of PPMI rate, which is even lower than the one observed post TAVR, whether Self-expandable or balloon expandable valves are used. Therefore, this rate should be considered as a benchmark when TAVR is offered to patients especially if they are intermediate or low risk candidates. Moreover, this less traumatic surgical technique may be retained whenever stent design modifications for TAVR are attempted.
References
- Klapkowski A, Pawlaczy kR, Kempa M, et al. Complete atrioventricular block after isolated aortic valve replacement. Kardiol Pol. 2016; 74: 985-993.
- Mehaffey JH, Haywood NS, Hawkins RB, et al. Need for permanent pacemaker after surgical aortic valve replacement reduces long-term survival. Ann thorac surg. 2018; 106: 460- 465.
- Lee MY, Yeshwant SC, Chava S, et al. Mechanisms of heart block after transcatheter aortic valve replacement-cardiac anatomy, clinical predictors and mechanical factors that contribute to permanent pacemaker implantation. Arryth electrophysiol rev. 2015; 4: 81-85.
- Nazif T, Dizon J, Hahn R, et al. Predictors and clinical outcomes of permanent pace maker implantation after transcatheter aortic valve replacement. JACC. 2015; 8: 60-69.
- Bagur R, Manazzoni J, Dumont E, et al. Permanent pacemaker implantation following isolated aortic valve replacement in a large cohort of elderly patients with severe aortic stenosis. Heart. 2011; 97: 1687-1694.
- Erdogan H, Kayalar N, Ardal H, et al. Risk factors for requirement of permanent pacemaker implantation after aortic valve replacement. J card Surg. 2006; 21: 211-215.
- Nardi P, Pellegrino A, Scafuri A, et al. Permanent pace maker implantation after isolated aortic valve replacement :Incidence,risk factors and surgical technique aspects. Journal of cardiovascular medicine. 2010; 11: 14-19.
- Dizon J, Nazif T, Biviano A, et al. New pacemaker implantation after surgical aortic valve replacement in the partner trials:Rates,Risk factors,and clinical outcomes. J Am Col Cardiol. 2018; 71: 308.
- Kawkabani N, Boustros O, Farah R, et al. Reproducible and Reliable Modified Technique of surgical aortic valve replacement that decreases the incidence of permanent pacemaker implantation. International journal of cardiothoracic and vascular Surgery. 2020; 6: 44-48.
- Hwang Y, Kim J, Hyun Lee J, et al. Conduction disturbance after isolated surgical aortic valve replacement in degenerative aortic stenosis. Thorac cardiovasc Surg. 2017; 154: 1556-1565.
- Matthews I, Fazal I, Bates M, et al. In patients undergoing aortic valve replacement, what factors predict the requirement for permanent pacemaker implantation. Interactive cardiovascular and thoracic surgery. 2011; 12: 475-479.